Hemodynamic Impact Of Retrograde Inner Branched Aortic Arch Endografts For Left Subclavian Artery Perfusion
William J. Yoon, MD1, Cheong Jun Lee, MD2, Kevin Mani, MD, PhD1, Anders Wanhainen, MD, PhD1.
1Uppsala University, Uppsala, Sweden, 2NorthShore University HealthSystem, Evanston, IL, USA.
OBJECTIVES: Retrograde inner branched endografts (RIBEs) for left subclavian artery (LSA) perfusion constitute a viable option for expanding the landing zone for TEVAR in the aortic arch. But its impact on LSA hemodynamics has not been widely described. We compared hemodynamic parameters in the LSA before and after RIBE implantation utilizing computational fluid dynamic (CFD) simulations.
METHODS: A disease-free aortic arch geometry extracted from publicly available de-identified CT scans were used to build two 3D geometric models using SimVascular software: Without-RIBE model (a native aortic arch) and With-RIBE model (Figure). These two models were then discretized into finite element meshes for CFD simulations. In-flow boundary conditions were prescribed using nominal pulsatile cardiac function. Outlet boundary conditions consisted of Windkessel models with previously published values. Rigid wall flow simulations were performed with incompressible Newtonian Navier-Stokes flow solver.
RESULTS: Peak and mean LSA flow rates were lower in the With-RIBE model simulation compared with the Without-RIBE model simulation (32.65 mL/s vs 38.74 mL/s, 10.51 mL/s vs 11.35 mL/s, respectively). Peak systolic and mean LSA pressures were also lower in the With-RIBE simulation (145.48 mm Hg vs 156.85 mm Hg, 119.29 mm Hg vs 122.98 mm Hg, respectively). Regardless of RIBE presence, time-averaged wall shear stress values (TAWSS) were within the physiologic range of 10 to 70 dynes/cm2. The With-RIBE model, compared to the Without-RIBE model, was associated with higher oscillatory shear index (OSI) and increased percentage of high OSI area (> 0.2) (0.089 vs 0.05, 13.78% vs 2.54%, respectively), which is known as an atherogenic condition. In addition, high OSI was observed where the low TAWSS (Figure), revealing an inverse relationship. These results suggest clinically relevant disturbed flows in the With-RIBE configuration compared to the Without-RIBE.
CONCLUSIONS: In this pilot study, case specific CFD modelling appears to be a viable method for assessing the hemodynamic change in the LSA after RIBE implantation. CFD simulations demonstrate geometry dependent and possibly clinically relevant flow disturbances following complex arch TEVAR, which could have important implications for monitoring and follow-up care after branched endovascular repair. 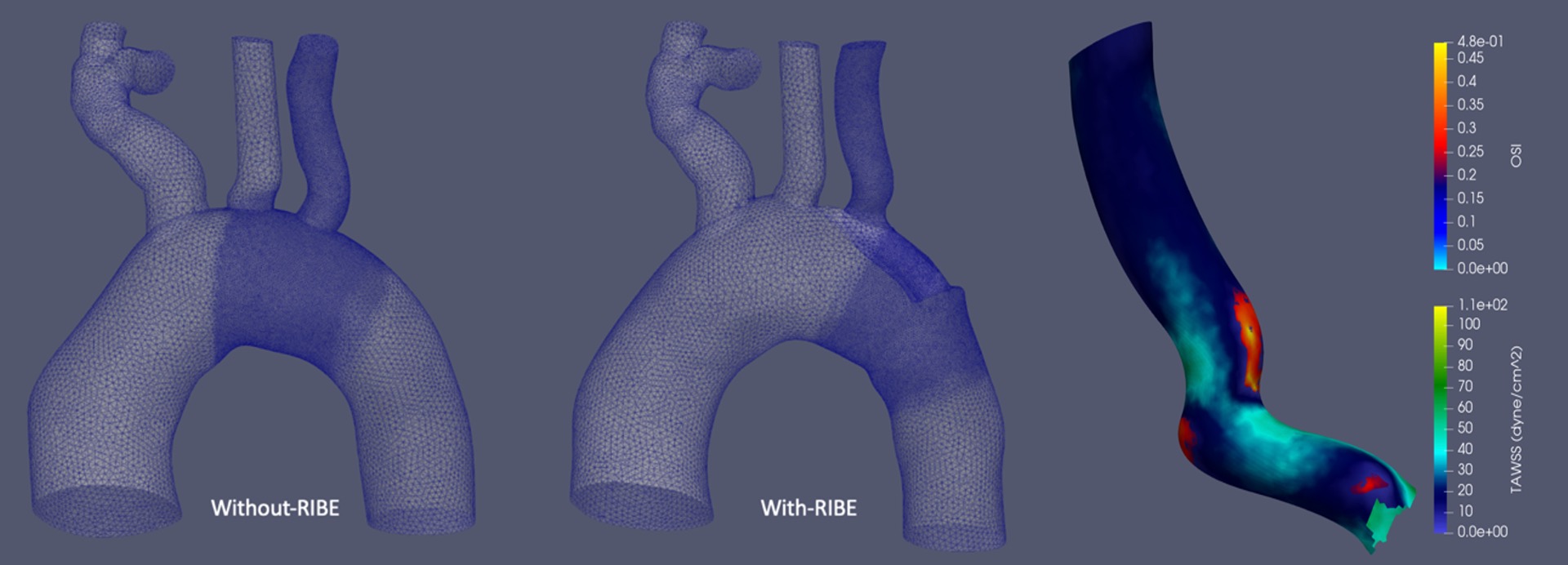
Back to 2022 ePosters
