Outcomes Of TEVAR For Chronic Type B Aortic Dissection In The Vascular Quality Initiative
Abhishek Devaguptapu Rao, BA/BS1, Ambar Mehta, MD MPH1, Priya B. Patel, MD MPH2, James Iannuzzi, MD MPH3, Karan Garg, MD4, Marc L. Schermerhorn, MD5, Jeffrey J. Siracuse, MD MBA6, Hiroo Takayama, MD PhD1, Virendra I. Patel, MD MPH1.
1Division of Cardiac, Thoracic, and Vascular Surgery, NYP-Columbia University Irving Medical Center, New York, NY, USA, 2Division of General Surgery, Rutgers-Robert Wood Johnson Medical School, Brunswick, NJ, USA, 3Division of Vascular Surgery, U California San Francisco School of Medicine, San Francisco, CA, USA, 4Division of Vascular and Endovascular Surgery, NYU School of Medicine, New York, NY, USA, 5Division of Vascular and Endovascular Surgery, Beth Israel Deaconess Medical Center, Boston, MA, USA, 6Division of Vascular and Endovascular Surgery, Boston University, Boston, MA, USA.
Objective:
TEVAR has increasingly been used for the treatment of uncomplicated and complicated chronic Type B aortic dissections (tB-Ad). Yet there exists limited national data evaluating outcomes and predictors of adverse events. We used prospectively collected data from the Vascular Quality Initiative (VQI) to evaluate the presentation and clinical features of chronic aortic dissections as well as outcomes following repair.
Methods:
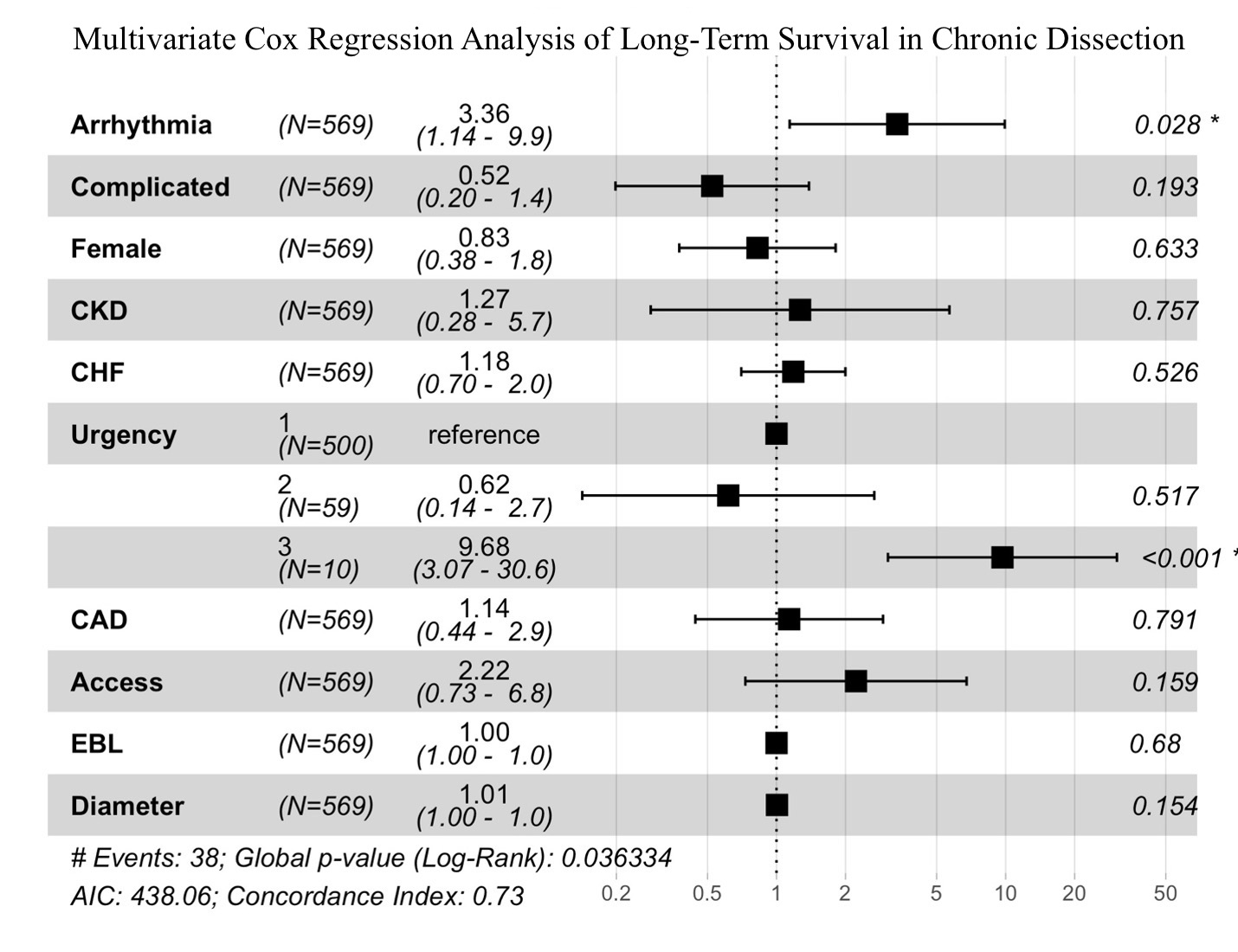
We queried the VQI database (2011-2020) for patients undergoing TEVAR for chronic (>12 weeks) tB-Ad, dichotomizing patients into uncomplicated versus complicated (visceral and limb malperfusion, rupture, or rapid expansion) dissections. Outcomes included 30-day mortality, perioperative complications, and three-year survival. Multivariable logistic regressions and Cox proportional hazard regressions accounted for confounding by adjusting for demographic and anatomic factors.
Results:
Of 569 patients treated for chronic Type B aortic dissection, 21% had complicated dissections which included expansion (16%), malperfusion (4.4%), and rupture (.84%). Complicated dissections were associated with longer procedural time (150min v. 130min, p<.01) and more often incorporated visceral vessels (3.9 v 3.2, p<.02). Complicated and uncomplicated dissections had similar unadjusted rates of mortality (0.9% vs. 2.6%, p=.48) and any complications (17% v. 13%, p=.26). Furthermore, 3-year survival was comparable among both groups (95% v. 89%, log-rank p=.19). After adjustment the following variables were independently associated with higher odds of 30-day mortality: CAD (OR 5.9 [95%-CI 1.0-30.0], P=.04), severe chronic kidney disease (OR 5.9 [1.4-43], P=.02), and emergent presentation (OR 28 [2.5-324], P<.01). Factors associated with decreased long-term survival included emergent repair (HR 9.7 [3.0-31], P<.01) and severe cardiac arrhythmia (HR 3.4 [1.1-10], P<.01).
Conclusions:
A significant number of patients undergoing TEVAR for chronic tB-Ad presented for aneurysmal degeneration of chronic dissection. Most patients undergoing TEVAR for chronic dissections have favorable outcomes; however, emergent clinical presentation is associated with higher procedural mortality and worse late survival. Further study is necessary to identify key risks for emergent presentation to implement clinical protocols and improve outcomes further.
Back to 2022 ePosters
