Open Revascularization For Acute Mesenteric Ischemia Is Associated With Increased Mortality When Compared To Endovascular Intervention
Blake E. Murphy, MD, Myra Ahmad, BA, Ameera Haq, BS, Elina Quiroga, MD, Benjamin W. Starnes, MD, Sara L. Zettervall, MD MPH.
University of Washington, Seattle, WA, USA.
Objectives: Historically, open approaches have been considered the primary treatment for acute mesenteric ischemia (AMI). However, the use of endovascular therapy is increasing. Given the paucity of current data, this study aims to compare outcomes between open and endovascular interventions for AMI. Methods: Patients who underwent open and endovascular revascularization for AMI between 2005-2018 were identified in the National Surgical Quality Improvement Program by ICD-9 and ICD-10 codes. Demographics, comorbidities, pre-operative laboratory values, and 30-day outcomes were compared between patient populations. A subgroup analysis was performed to compare operative approaches among those with and without concomitant bowel resection to account for severity of disease. Multivariable analysis was utilized to adjust for differences between groups. Results: A total of 785 patients underwent revascularization for AMI (699 open (89%), 86 (11%) endovascular). 347 (44%) underwent embolectomy, 266 (34%) underwent mesenteric bypass, 86 (11%) underwent thromboendoarterectomy, 80 (10%) underwent angioplasty, atherectomy, or stenting, and 6 (0.8%) underwent pharmacomechanical thrombectomy. During revascularization, 283 (36%) patients had concomitant bowel resections, (246 (35%) open, 37 (43%) endovascular). Patients who underwent endovascular repair were older (70 years vs. 68 years, p<0.001). Other comorbidities and pre-operative lab values were similar between groups. When outcomes were assessed, 30-day mortality (32% vs 16% p=0.002) and respiratory failure (38% vs 26%, p=0.022) were higher following open repair. All other outcomes were similar (Table 1). Following adjustment, these findings remained significant (30-day-mortality: OR 2.6, 95% CI: 1.4-5.0; respiratory failure: OR 1.7, 95% CI: 1.0-2.9). When patients who underwent bowel resection were assessed separately, 30-day mortality (OR 2.8, 95% Cl: 1.0-7.4) remained higher following open repair. For patients without bowel resection, 30-day mortality (OR 3.3; 95% CI: 1.2-2.8) and respiratory failure (OR 3.2, 95% CI: 1.2-8.4) were also higher following open revascularization. Conclusions: After accounting for disease severity, open revascularization for AMI is associated with higher perioperative morbidity and mortality when compared to endovascular intervention. Given these data, the need for bowel resection should not preclude endovascular treatment for AMI. Rather, endovascular techniques for revascularization should be considered in appropriately selected patients. 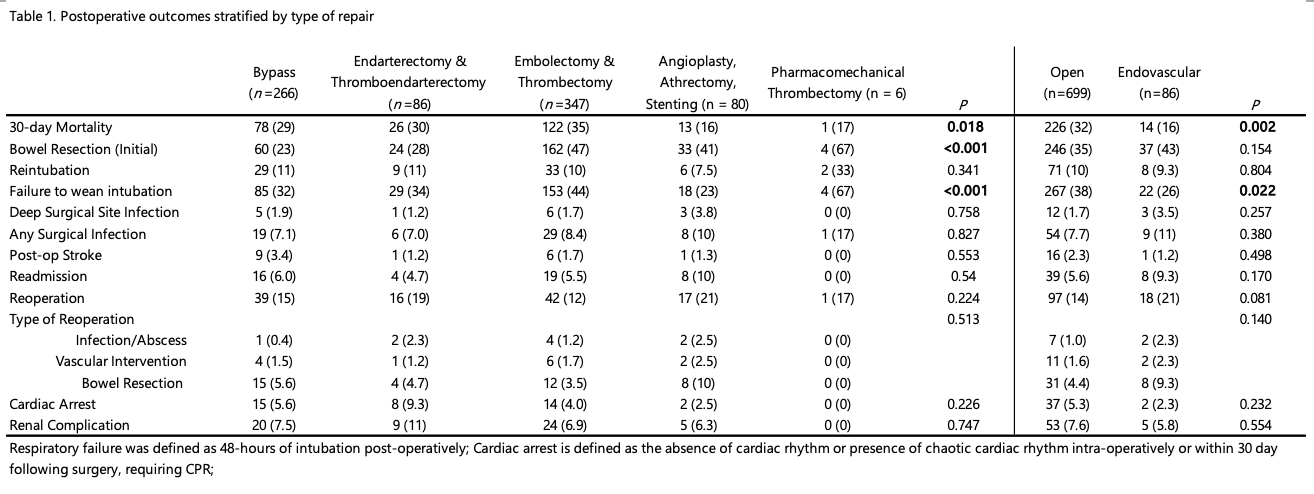
Back to 2022 ePosters
