Outcomes Of Open Abdominal Aortic Aneurysm Repair In Patients With Previous EVAR
Donna Bahroloomi, MD, Khalil Qato, MD, Nhan Nguyen, Sasha Suarez, Deanna Schreiber-Gregory, Allan Conway, MD, Gary Giangola, MD, Alfio Carroccio, MD.
Lenox Hill Hospital, New York City, NY, USA.
Objectives: Due to failure of Endovascular repair of abdominal aortic aneurysm (EVAR) over time, there has been an increasing rate of open surgical re-intervention. This study aims to compare postoperative outcomes of patients who undergo open repair of abdominal aortic aneurysm (OAR) to those undergoing OAR with history of previous EVAR (EVAR-c).
Methods: A retrospective study of the Vascular Quality Initiative (VQI) database was conducted for patients who underwent OAR between 2013-2021. We included all patients who underwent OAR, comparing two groups: those with no prior intervention and those with prior EVAR. Demographic data, comorbidities, and operative details were analyzed. Patients who had prior open aortic surgery were excluded. Primary endpoint was in-hospital mortality. Sub-group analysis was performed for patients who underwent elective repair.
Results: 13,464 patients were included in the study. 881 (6.5%) patients were in the EVAR-c and 12,583 (93.5%) in the OAR group. The average age was 69.8 (±8.8) years and 9,938 (73.8%) of patients were male. The average aortic diameter was 63.6 ±17.7mm. 70.9% (n=9543) were treated electively, 11.8% (n=1588) were symptomatic and 17.3% (n=2322) were ruptured. On univariate analysis, the EVAR-c group had a higher rate of in-hospital mortality (10.7% vs. 8.7%, p=.05) and post-operative complications (53.2% vs 42.5%, p<.0001). Multivariate analysis of factors that contributed to mortality include procedure time (p<.04), proximal clamp position (p<.0001), and estimated blood loss (EBL; p<.0001). Symptomatic and rupture patients also contributed to mortality (p<.001). In the elective setting, univariate analysis showed an increase in mortality in EVAR-c patients (p<.0001). Factors contributing to mortality on multivariate analysis were EBL (p<.0001) and procedure time (p<.001). Proximal clamp position was not a statistically significant contributor to in-hospital mortality (p=0.2) but was a significant contributor to post-operative complications (p<.0001).
Conclusion: When compared to patients undergoing OAR without previous intervention, patients undergoing EVAR-c in both the general and elective setting have higher in-hospital mortality and postoperative complications. Proximal clamp position did not impact mortality in elective setting. Further studies are needed to determine potential improvement in mortality with earlier open repair of EVAR-c patients in the elective setting. 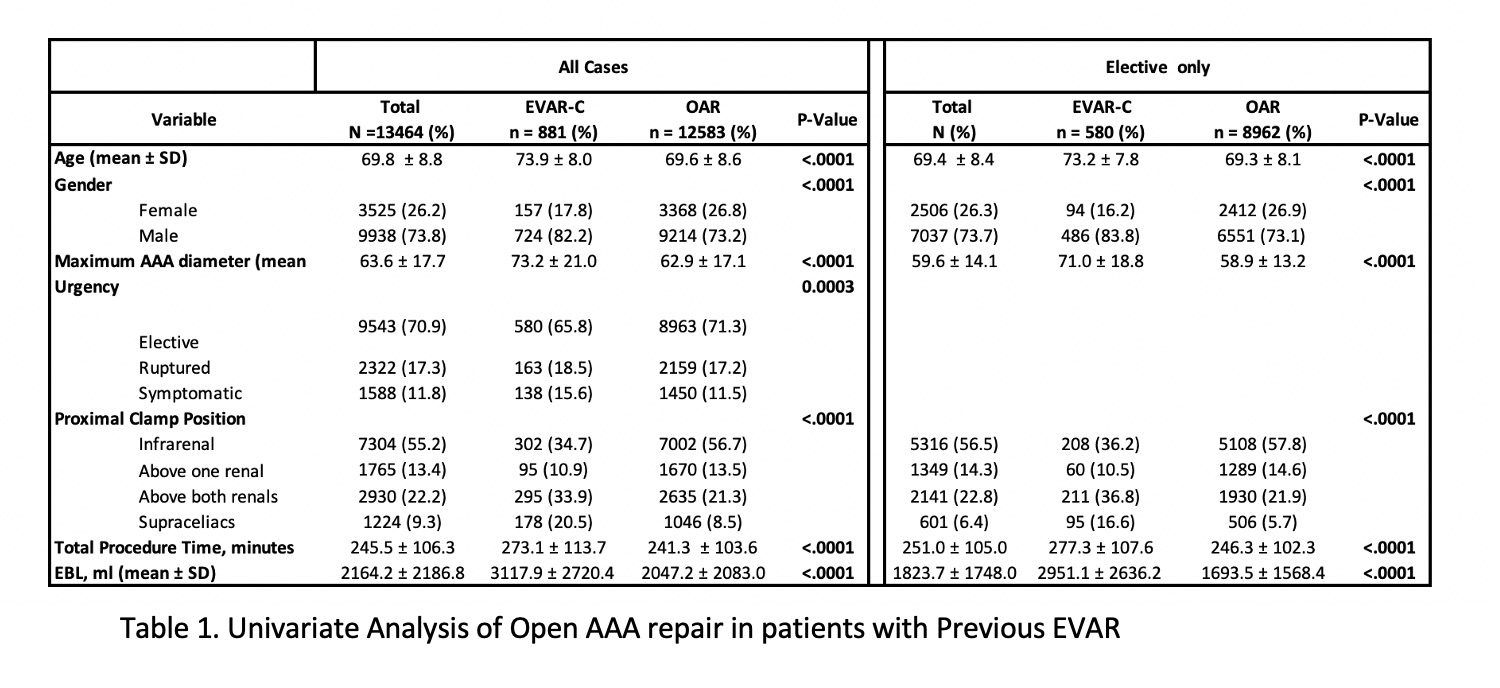
Back to 2022 ePosters
