TEVAR Outcomes For Type B Dissection And Thoracic Aortic Aneurysm
Peter V. Cooke, BA1, Justin M. George, MD2, Halbert Bai, MPH1, Windsor Ting, MD2, Ajit Rao, MD2, Michael L. Marin, MD1, Peter L. Faries, MD1, Rami O. Tadros, MD1.
1Icahn School of Medicine at Mount Sinai, New York, NY, USA, 2Division of Vascular Surgery, Mount Sinai Hospital, New York, NY, USA.
OBJECTIVES: The most common indications for thoracic endovascular aortic repair (TEVAR) are thoracic aortic aneurysm (TAA) and type B aortic dissection (TBAD). The objective of this study is to compare complications, reintervention rates, and short-term mortality in patients undergoing TEVAR for TBAD versus TAA.
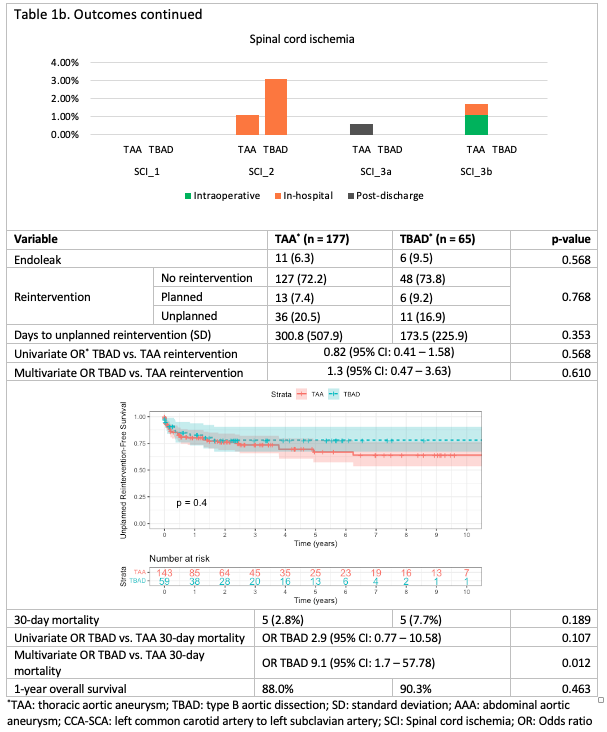
METHODS: A prospectively maintained single-institution database was retrospectively reviewed for patients undergoing TEVAR from August 2001 to January 2020. Patients were stratified into two cohorts based on TEVAR indication: TBAD and TAA. TBAD patients with concomitant TAA were placed in the TBAD cohort. Spinal cord ischemia was classified from grade 0 - 3b and other complications were categorized as ‘mild’, ‘moderate’, and ‘severe’ based on SVS guideline classification standards.
RESULTS: 242 patients underwent TEVAR, 177 for TAA and 65 for TBAD. The TAA cohort was older (mean age 72.4 vs.6.5;p<0.001), had a higher prevalence of known AAA history (26.6%vs.10.0%;p = 0.023) and CAD (47.5%vs.26.2%;p =0.005) but a lower prevalence of obesity (23.2%vs.51.9%;p=0.001) and CKD (15.3%vs.20.0%;p=0.011). The cohorts also differed in terms of ethnicity (p=0.004). The TAA cohort was less likely to undergo prophylactic carotid to subclavian bypass (9.6%vs.41.5%,p<0.001). Intraoperative, in-hospital, and post-discharge complication rates are featured in Table 1. Four (2.3%) TAA patients experienced grade 3 spinal cord ischemia versus 0 (0%) TBAD patients (p=0.282). The thirty-day reintervention rate did not differ significantly (p=0.270). The odds of reintervention also were not significantly different, both on univariate and multivariate analysis (p=0.568,610, respectively). Log-rank test revealed no difference in reintervention-free survival (p=0.22).While on univariate analysis, 30-day mortality was not significantly different between cohorts (p=0.107), on multivariate analysis, TBAD patients had a higher likelihood of 30-day mortality OR 9.1 (95% CI: 1.7 - 57.78). One-year overall survival for TAA and TBAD patients was 88.0% and 90.3%, respectively (p=0.463).
CONCLUSIONS: TBAD and TAA patients treated with TEVAR differed in terms of patient characteristics and outcomes. Most notably, TBAD patients had higher odds of mortality within 30 days of TEVAR on multivariate analysis. 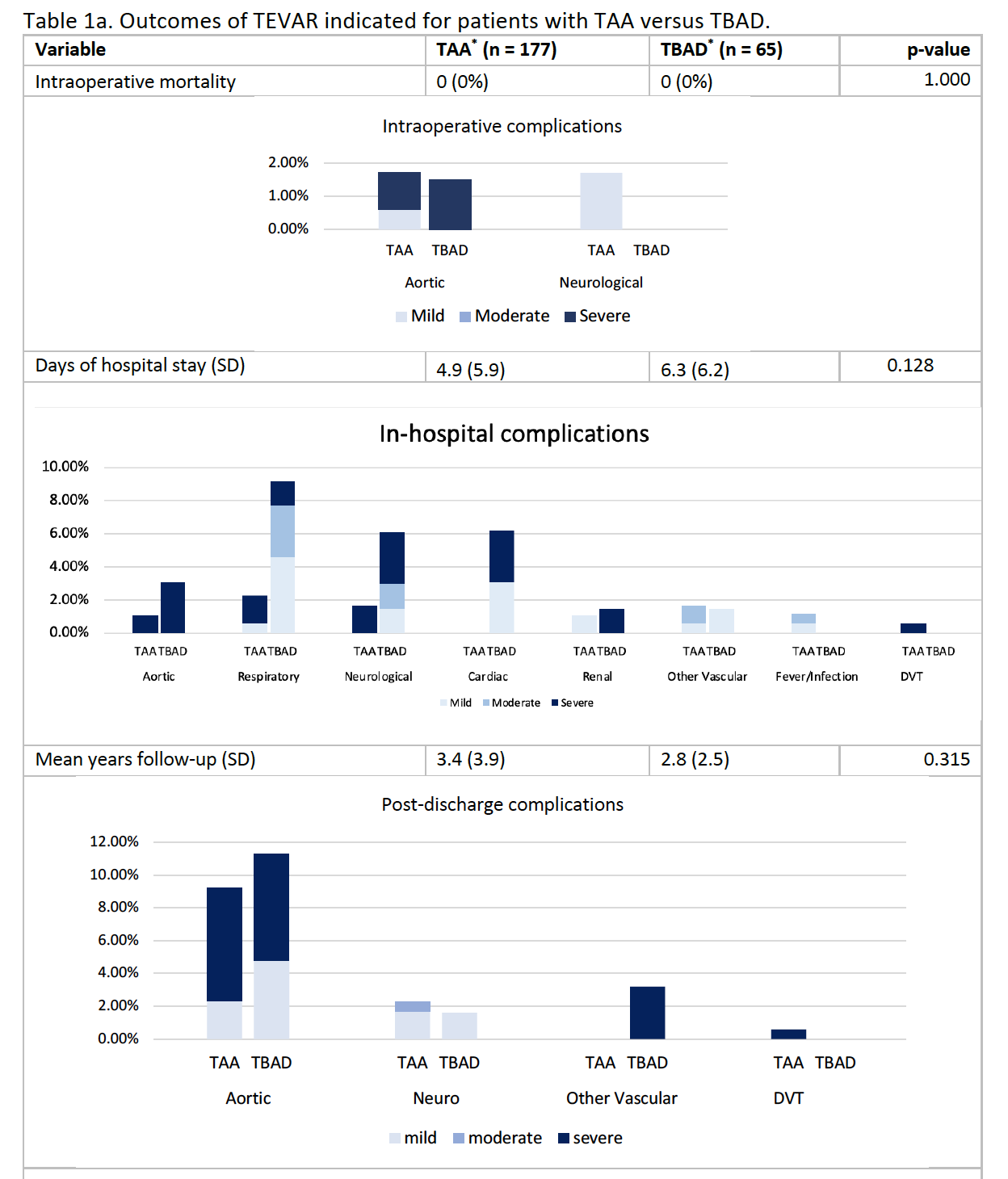
Back to 2022 ePosters
