Risk Profile For Low-dose Anticoagulation Therapy With Rivaroxaban And Apixaban In A Veteran Based Population
Sonia Lele, Ashwin Ghadiyaram, James Dittman, Diana Otoya, MD, Kedar Lavingia, Michael F. Amendola, MD.
VA Medical Center/VCU Health System, Richmond, VA, USA.
INTRODUCTION: Xarelto (X; Rivaroxaban) and Eliquis (E; Apixaban) are two oral Factor 10A inhibitor anticoagulants commonly used to prevent coagulation and embolism events in patients with vascular disease. Despite the protective effects of these medications even at low doses, there still exists the risk of hemorrhages and thrombus formation in patients on these medications. We predict that these two anticoagulants exhibit significantly different risk profiles for these complications.
METHODS: After obtaining IRB approval, a Veterans Administration Anticoagulation Therapy database over an approximate six-month period (December 5, 2020 to June 3, 2021) at the Central Virginia VA Health Care System in Richmond, VA was accessed. Patients were stratified based on use of either low dose Xarelto or Eliquis. Patients were followed for outcomes ranging from the start date to the end date of anticoagulation therapy for each patient. Patients currently still on anticoagulation therapy were followed until July 1, 2021. Outcomes examined were bleeding events, thrombosis, and death. Risk factors examined prior to the start of anticoagulation therapy were diabetes mellitus, coronary artery disease, myocardial infarction, smoking, hypertension, number of antihypertensive drugs, acute limb ischemia, peripheral vascular disease, heart failure, atrial fibrillation, transient ischemic attack, cerebrovascular accident, aspirin usage, Plavix (clopidogrel) usage, beta blocker usage, statin usage, and GFR. Unpaired t-tests* and Chi-Squares** were utilized to assess cohort differences. Binary logistic regression was utilized to evaluate predictors of complications related to the anticoagulation medications utilized.
RESULTS: There were 18 patients undergoing X therapy and 72 on E. There was no statistically significant in terms demographics when comparing X to E except PVD (88.8% v. 22.2%; p=0.0001**), atrial fibrillation (0% v. 40.2%; p=0.0005**), aspirin (94.4% v. 45.8%; p=0.0001**) and Plavix (44.4% v. 13.9%; p=0.007**).
CONCLUSION: In review of two common oral Factor 10A inhibitors found similar thrombosis and bleeding events in our veteran population. Eliquis was more commonly used in our center with longer mean duration of therapy. These data continue to support the use of these types of medications for patients with vascular disease. 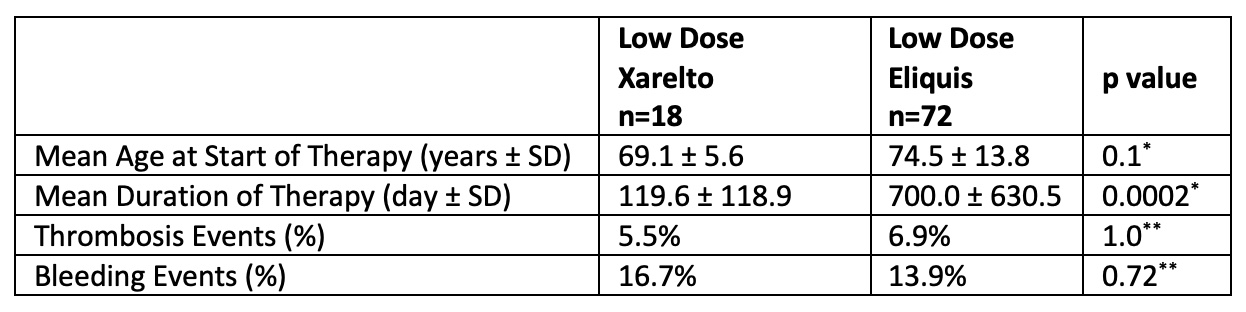
Back to 2022 ePosters
