Living In A Food Desert Does Not Negatively Impact Arteriovenous Graft Outcomes.
Sonia Lele, Diana Otoya, MD, Kedar Lavingia, MD, Michael Amendola, MD.
VA Medical Center/VCU Health System, Richmond, VA, USA.
OBJECTIVES:
Food deserts have been defined as poor access to healthy food options and can lead to numerous metabolic risks. Previous studies have demonstrated food deserts are associated with increased wound complications post operatively. We hypothesized that similar to previous studies, living in a food desert (FD) will be associated with increased arteriovenous graft complications.
METHODS: A Veterans Administration Hospital dialysis access database was analyzed over a four-year period (May 2014 to December 2018) to identify all patients who had AVG placement. Clinical records were also examined for patient address, past medical history, medications, pre-operative labs, and clinical outcomes, including infection rates, successful cannulation, functional patency (successful needle cannulation and usage on dialysis), thrombosis events, and endovascular interventions per access. Food desert (FD) was defined using US Department of Agriculture’s Food Access Research Atlas. All outcomes were followed until July 2021. Student’s t-test** and Fisher’s Exact test* were utilized.
RESULTS: A total of 89 AVG were placed (1 patient was excluded due to lack of address). A minority (n=17, 20%) lived in a FD. Comparing FD compared to Non-FD patients, there was no difference in infection rates (5.9% vs. 28.2%; p=0.06*), functional patency (805 ± 524 vs. 577 ± 538; p=0.12**), thrombosis rates (1.8 ± 2.2 vs. 1.2 ± 1.8; p=0.24**) nor the endovascular interventions per access (3.4 ± 4.7 vs. 2.4 ± 3.5; p=0.32**) respectively. FD patients had 100% cannulation rates compared to 76.1% in Non-FD (p=0.03*). Baseline demographic factors were not statistically significant between the two groups.
CONCLUSIONS: Contrary to previous studies, living in a food desert was not associated with increased rate of infection, functional patency, thrombosis events, or endovascular interventions. Cannulation rates were found to be higher within the food desert group. Further studies are needed to assess food access impact on hemodialysis access outcomes. 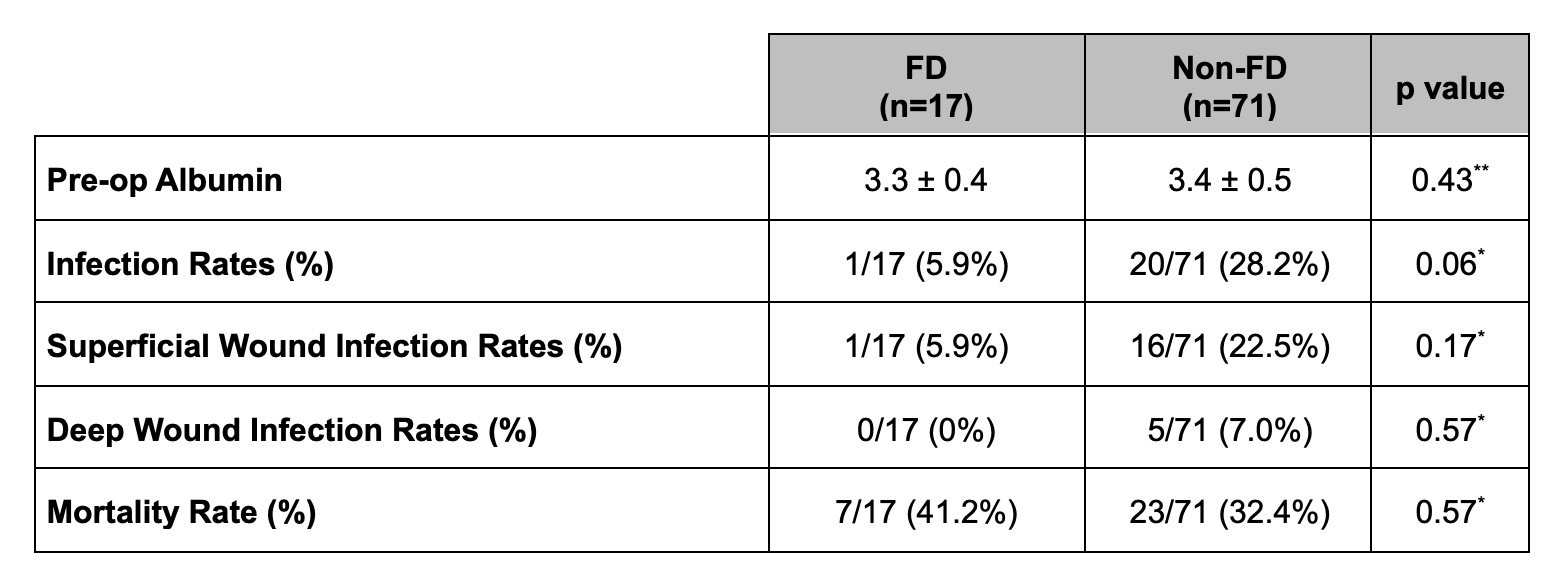
Back to 2022 ePosters
