Enhanced Recovery After Surgery (ERAS) Protocol Decreases Hospital Length Of Stay And Post-operative Opioid Use For Thoracic Outlet Syndrome Surgical Decompression
Kenneth M. Rosenberg, PhD, David N. Blitzer, MD, Sarah Rosenberger, CRNP, Rajabrata Sarkar, MD, PhD.
University of Maryland School of Medicine, Baltimore, MD, USA.
OBJECTIVES: Thoracic outlet syndrome (TOS) is a complex disease process that often results in disabling pain and weakness in the upper extremities or vascular complications. For patients unresponsive to non-operative measures, surgical therapy provides definitive relief but is associated with inpatient hospital stay and post-operative pain. We hypothesized that implementing an enhanced recovery after surgery (ERAS) protocol, including multimodal pain management, would reduce post-operative narcotic use and hospital length of stay (LOS).
METHODS: This study was a retrospective case control study comparing three periods of post-operative care: 1) conventional perioperative and pain management, 2) routine implantation of ropivacaine pump, and 3) formal ERAS perioperative protocol including ropivacaine pump. The study was conducted at a single tertiary hospital and included patients undergoing TOS decompression for any etiology during 2016-2021. The primary outcomes included LOS and inpatient opioid use (morphine equivalents).
RESULTS: We collected data from 90 patients (97 total surgeries) who underwent first rib resection during the evaluation period. Comparing conventional vs. multimodal pain management, both LOS and opioid use significantly decreased. LOS was shorter for the multimodal group (Conventional: 3.27 [2.53,3.45] vs. Multimodal: 2.26 [1.39,3.33], P<0.001) and daily morphine equivalents were significantly less (Conventional: 34 [22,53] vs. Multimodal: 11 [7,18], P<0.001). Focusing specifically on the multimodal group, we observed significant differences in outcomes for multimodal pain management alone (n=27) vs the full ERAS protocol (n=17). LOS was shorter for ERAS patients (Multimodal alone: 2.35 [2.17,3.38] vs. ERAS: 1.51 [1.31,2.26], P<0.05); however, there was no difference in opioid use (Multimodal alone: 13 [8,17] vs. ERAS: 11 [6,18], P>0.05). There were no significant differences in our secondary outcomes for either comparison (table).
CONCLUSIONS: Our data show multimodal pain management decreases opioid requirement and hospital stays, suggesting an acceleration in patientsí comfort and confidence that their pain can be managed at home. Consistent with other areas of surgery, ERAS yielded a further decrease in LOS, indicating additional factors that can positively impact postoperative recovery. These combined perioperative measures decreased hospital stay by >50% and opioid use by 67%, greatly reducing resource utilization and improving early and safe discharge. 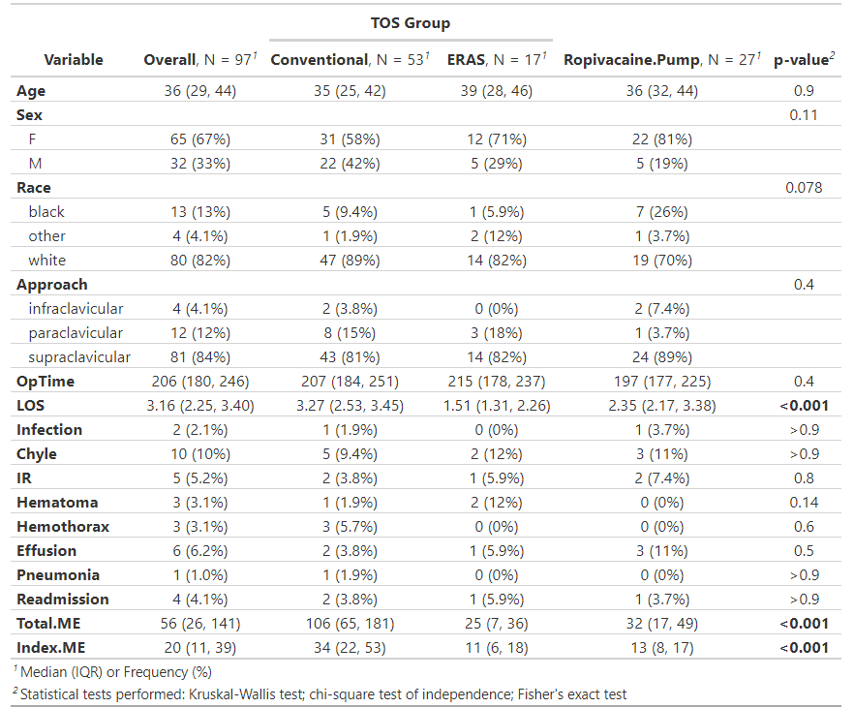
Back to 2022 ePosters
