Evidence Of Multi-modality Imaging Techniques To Characterize Chronic Total Occlusions In Critical Limb Ischemia Patients
Kavya Sinha, MD1, Christof Karmonik, PhD2, Alan Lumsden, MD1, Trisha Roy, MD, PhD1.
1Houston Methodist, Houston, TX, USA, 2Houston Methodist Academic Institute, Houston, TX, USA.
OBJECTIVES:Percutaneous vascular interventions (PVI) are widely recognized as the preferred treatment option for peripheral arterial disease (PAD). Not all lesions are amenable to PVI, but it is currently impossible to predict which patients will fail PVI in advance as it is guided using x-ray fluoroscopy, which suffers from limited soft-tissue contrast. MRI is a non-invasive imaging method that can produce high-quality maps of the peripheral vasculature and can characterize the composition of vascular lesions. The goal of this study was to develop a clinically feasible MRI method that could be used to help vascular surgeons to identify PAD lesions amenable to PVI.
METHODS:Sixteen patients with critical limb ischemia (CLI) underwent amputation, (2 below-knee amputations and 14 above-the-knee amputations). All images were acquired at the clinical 7T MRI scanner or the 3T MRI with the knee coil. Lesions were harvested (popliteal artery in 14 patients, peroneal in 1, and the trifurcation and TP trunk in the remaining subject) and were segmented into 1-2 cm samples stored in formalin. MicroMRI (9.4 T Bruker) and micro-CT (40μm) images were acquired to identify calcified lesion components and for direct comparison with the near in-vivo MRI images. RESULTS: In all subjects, 7T MRI yielded artifact-free, high-resolution images of superior contrast of the PAD lesions of interest with much-improved differentiation power than the corresponding computed tomography (figure 1). Calcified components could readily be appreciated in the UTE images. Comparison with the T1-weighted images allowed identification of collagen-rich regions compared to solid calcification.
CONCLUSIONS:
Clinical MRI using T1W, T2W, and UTE imaging can be used to characterize popliteal and tibial peripheral artery lesions. Ex-vivo imaging supported findings and initial impression of the MRI images. Future work will determine if this method can be used to predict success in peripheral endovascular interventions. 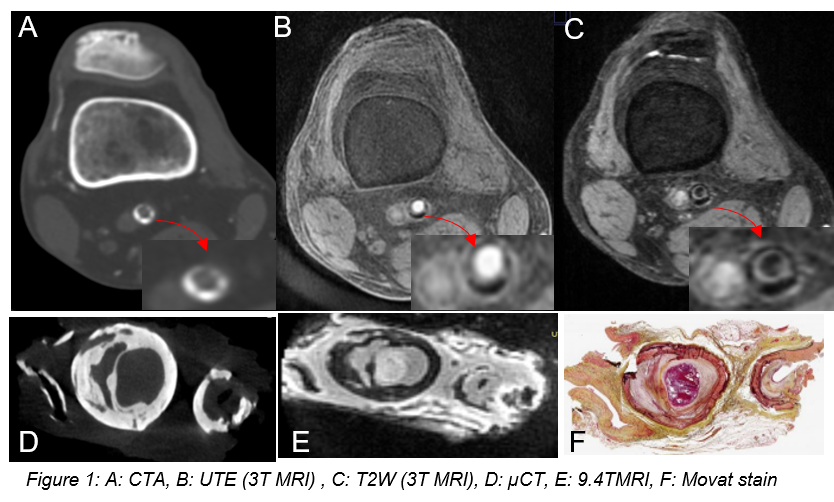
Back to 2022 ePosters
