Needle-fenestration Of Covered Stent-graft To Salvage Inadvertent Stent Misdeployment
Alex Intagliata, MHA, Kaitlyn M. Rountree, DO, Todd R. Vogel, MD, Naveen Balasundaram, MD, Jonathan Bath, MD.
University of Missouri, Columbia, MO, USA.
Demographics: Lower extremity peripheral artery disease (PAD) affects 8.5 million people in the United States, and is the third leading cause of atherosclerotic morbidity. As technology advances and the population ages, the number of minimally invasive, cost-effective endovascular procedures is increasing, and so too are the rates of complications. Even experienced providers can be plagued by unexpected complications requiring advanced techniques for procedure salvage. We present a case of endovascular recanalization of the superficial femoral artery (SFA) complicated by inadvertent distal stent deployment into a geniculate artery and a creative strategy for procedural rescue.
History: The patient is a 69-year-old man with rest pain who underwent SFA recanalization with Viabahn (W.L.Gore, AZ) covered stents. The stents extended from the SFA origin to the P2 segment of the popliteal artery for a length of 45cm. During completion angiography, the distal stent was discovered to have deployed into an anterior geniculate branch, not the intended popliteal target (Panel A, B). Additional imaging demonstrated the large collateralís trajectory superimposed on the true target.
Plan: We initially attempted to use a small balloon inflated distal to the stent to accordion this back into the popliteal artery but were unable to do so. Consequently, we utilized an Outback re-entry device (Johnson & Johnson, NJ) to pierce through the covered stent posteriorly and re-enter the true lumen of the popliteal artery (Panel C), placed a new guidewire distally into the posterior tibial artery and used cutting balloons to dilate the fenestration in the Viabahn. We then deployed an additional 6 x 50 mm Viabahn stent bridging from behind knee popliteal artery into the previous Viabahn stents (Panel D). Completion angiography (Panel E) demonstrated no evidence of distal embolization and the patient underwent an uncomplicated recovery. At one year follow-up, the stents are widely patent and the patient maintains symptomatic relief.
Discussion: This case highlights a creative technique for endovascular salvage of a potentially disastrous complication during SFA recanalization with covered stent-grafts utilizing an Outback re-entry device to needle-fenestrate the Viabahn stent allowing for balloon dilation and stenting into the P3 segment of the popliteal artery. 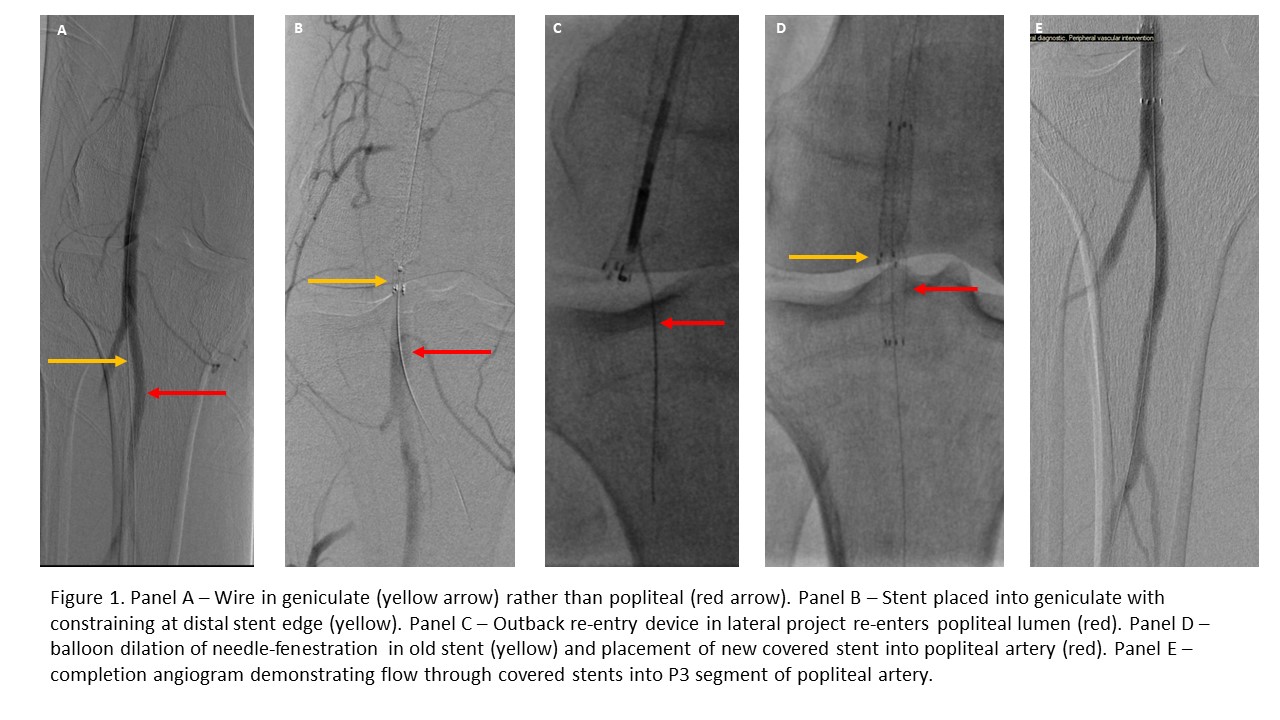
Back to 2022 Abstracts
