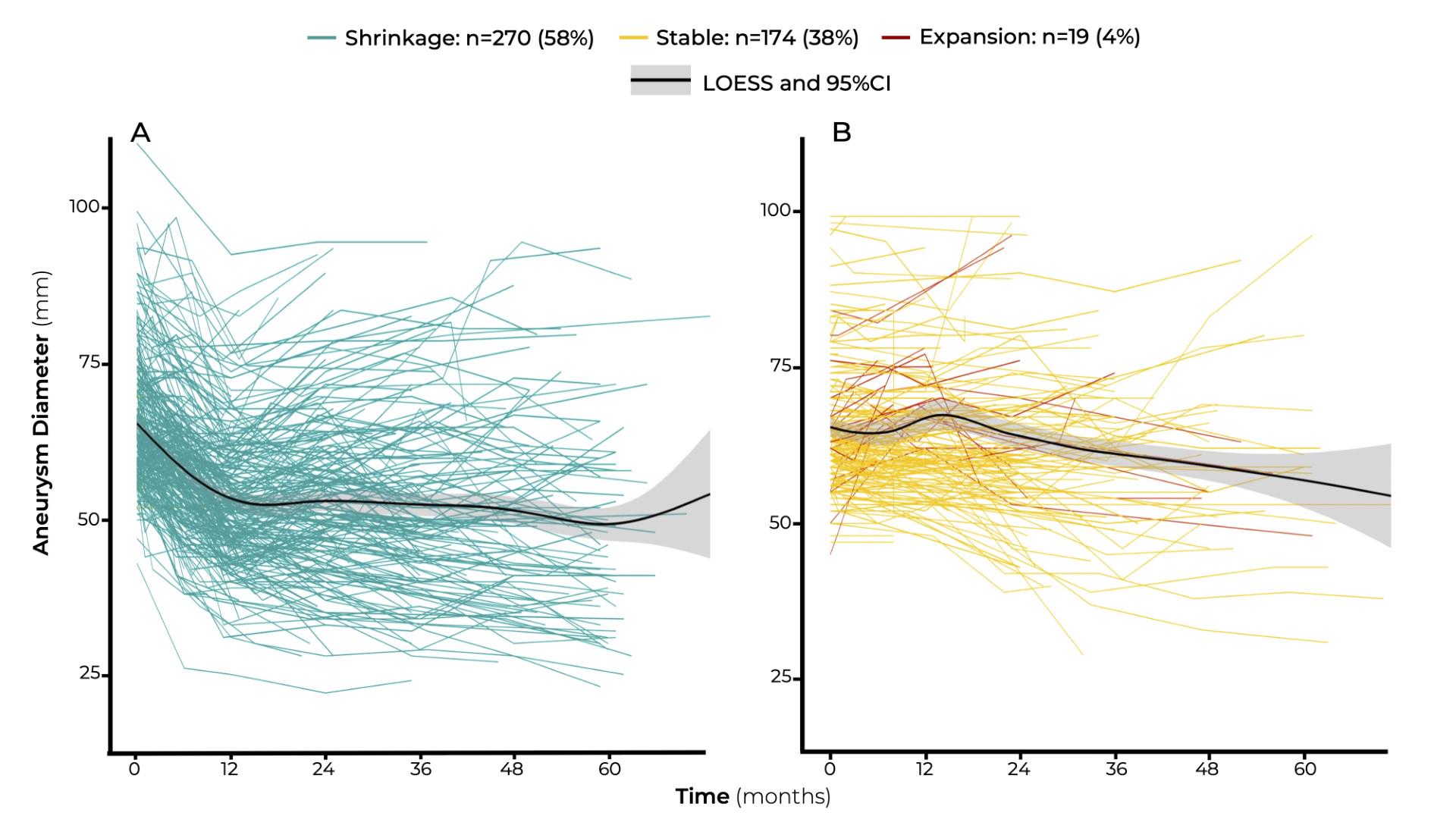
Objectives: To investigate the impact of early changes in aneurysm sac diameter on patient survival after fenestrated-branched endovascular repair (FB-EVAR) for complex abdominal (CAAA) or thoracoabdominal aortic aneurysms (TAAA).Methods: We reviewed the clinical data of patients enrolled in a prospective non-randomized study investigating FB-EVAR (2013-2022). Aneurysm sac diameters were measured from CT scans preoperatively and during follow-up. Maximum aortic diameter at 1-year (6-18 months) was compared to the early postoperative measure CTA (≤30 days). Patients were classified according to early sac dynamic into sac shrinkage (≥5mm) or failure to regress (<5mm or expansion). Primary endpoint was all cause survival, and secondary endpoints were cumulative incidences of aortic-related mortality (ARM), aneurysm rupture and aorta-related secondary intervention.Results: There were 549 patients treated by FB-EVAR. Of these, 463 patients (84%; 71% males; mean age 74±8 years-old) had > 1-year follow up (135 CAAAs, 328 TAAAs). Sac shrinkage at 1-year was observed in 270 patients (58%), sac expansion accounted for 4% of the entire cohort with no significant difference between patients with CAAAs and TAAAs (P>.05). Patients from both groups had similar cardiovascular risk factors, except for younger age among patients with sac shrinkage (73±8 vs. 75±8 years-old; p<.001). Median follow-up was 38 months (18-51). Survival estimates adjusted for confounders (age, chronic pulmonary disease, heart failure, dialysis, and aneurysm extent) revealed a higher hazard of late mortality in failure to regress patients (adjusted hazard ratio, 1.73; 95% Confidence Interval, 1.18-2.53; P=.005). Cumulative incidences of ARM (1.1% vs. 1.4%, p=.30) and aneurysm rupture (0.6% vs. 0.8%, p=.20) at 4-years were both comparable in patients with and without sac shrinkage. The sac behavior at 1 year had no predictive value for aorta-related secondary intervention (HR=3.84 95%CI (0.35-42.46); p=.259). The temporal trend of sac dynamic in both group is presented in Figure 1. Conclusions: Aneurysm sac shrinkage at 1-year is frequent after FB-EVAR and is associated with improved patient survival, while sac enlargement affects only a minority of patients. The low incidences of ARM and aneurysm rupture indicate that failure to regress is a surrogate marker for non-aortic causes of death.