Objective: To investigate which preoperative factors are most impactful on the 5-year survival of patients undergoing fenestrated/branched endovascular aortic repair (F/BEVAR) and to identify modifiable elements that, if time allows, should be actively managed and adequately controlled preoperatively.
Methods: Patients treated for complex anatomy aortic aneurysms using either a custom-manufactured or an off-the-shelf device were included. The exposure of interest was aneurysm type (group1-types I-III thoracoabdominal (TAAA) aneurysms vs group2-type IV TAAA vs group3-juxtarenal or suprarenal aneurysms) and the primary outcome was 5-year risk of all-cause mortality. Generalized linear models were used to estimate the crude 5-year risk of death in each group and the 5-year risk of death across groups. Each preoperative factor was added to the model individually and a change in estimate was calculated between the new risks and the crude risk. Preoperative factors with a change of estimate of ≥10% were utilized to create inverse probability of treatment weights for multivariable analysis.
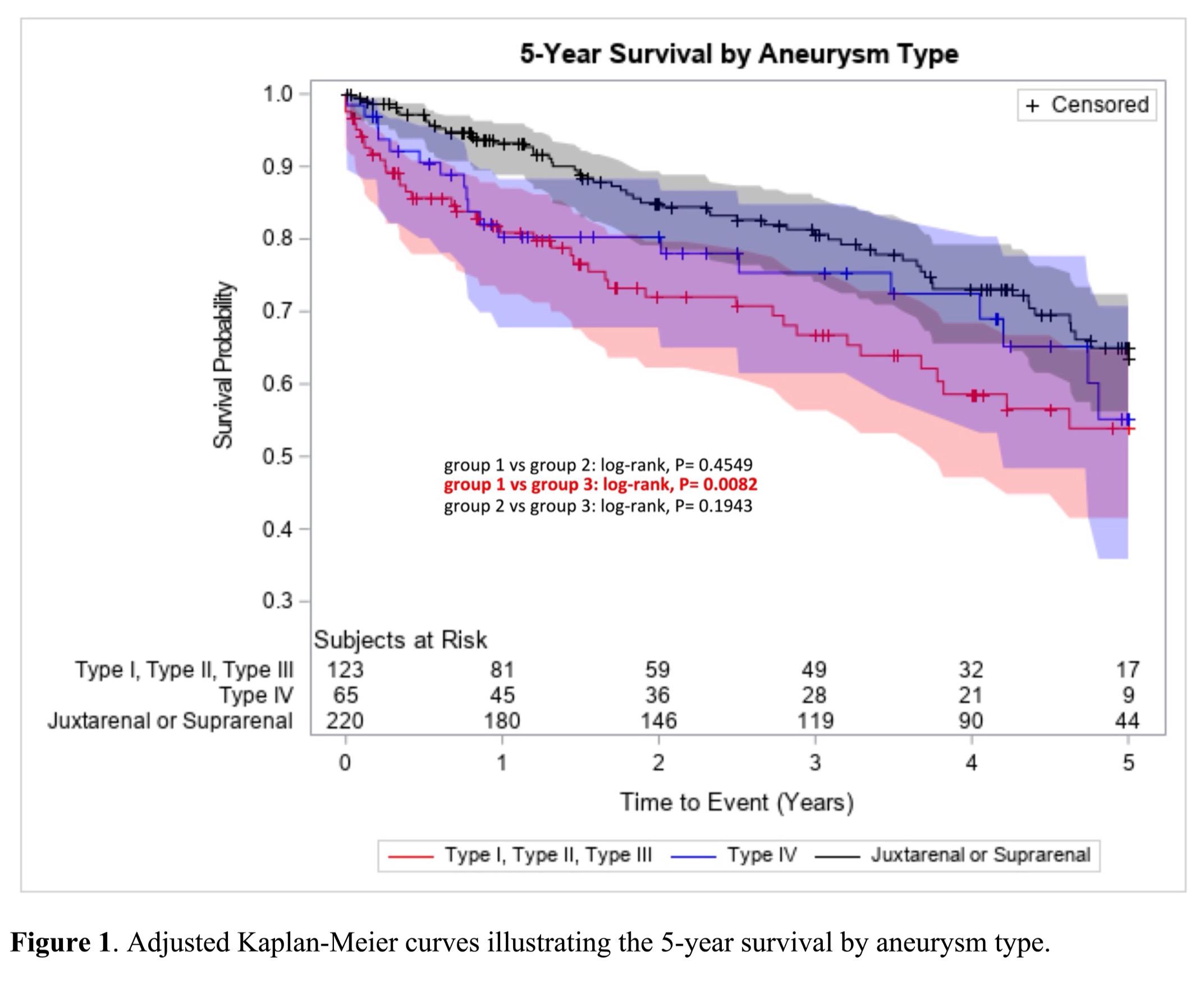
Results: 408 F/BEVAR patients were included, who were 71.6% male (mean age: 72.0±7.9 years). Ten of 21 preoperative factors analyzed had a change in estimate ≥10% (Table I). The greatest changes in estimates were observed for history of chronic heart failure, BMI≥30, and arrhythmia. Almost 60% of patients with CHF in group1 died within 5 years. Current smoking or overweight at the time of F/BEVAR increases the 5-year risk of death more significantly than having a history of myocardial infarction. After adjustment, patients in group1 had a significantly higher risk of 5-year all-cause mortality compared to those in group3 (Figure1, log-rank p-value=0.0082).
Conclusions: These findings suggest that cardiac pathologies are relevant preoperative elements that impact the 5-year survival post F/BEVAR. More specifically, CHF and arrhythmias should be used to alter patient selection and identify those patients more likely to benefit from repair. Moreover, modifiable risk factors such as weight loss and smoking cessation before F/BEVAR and during the surveillance period, might improve survival in this population.