OBJECTIVE: The recent publications of randomized trials comparing open bypass surgery to endovascular therapy in CLTI patients, BEST-CLI and BASIL-2, have resulted in potentially contradictory findings. The trials differed significantly regarding anatomic disease criteria as well as their primary endpoints. We perform an analysis of BEST-CLI patients with significant infrapopliteal disease undergoing open tibial bypass or endovascular tibial interventions to formulate a more precise comparative study for BASIL-2.
METHODS: BEST-CLI patients in Cohort 1 (adequate saphenous vein conduit) who had significant infrapopliteal disease and underwent tibial level intervention were included. Patients were randomized to bypass or endovascular therapy with a stratification that included the presence or absence of infrapopliteal disease. The primary outcome was major adverse limb events (MALE) or all-cause death. MALE included any major limb amputation or major re-intervention.
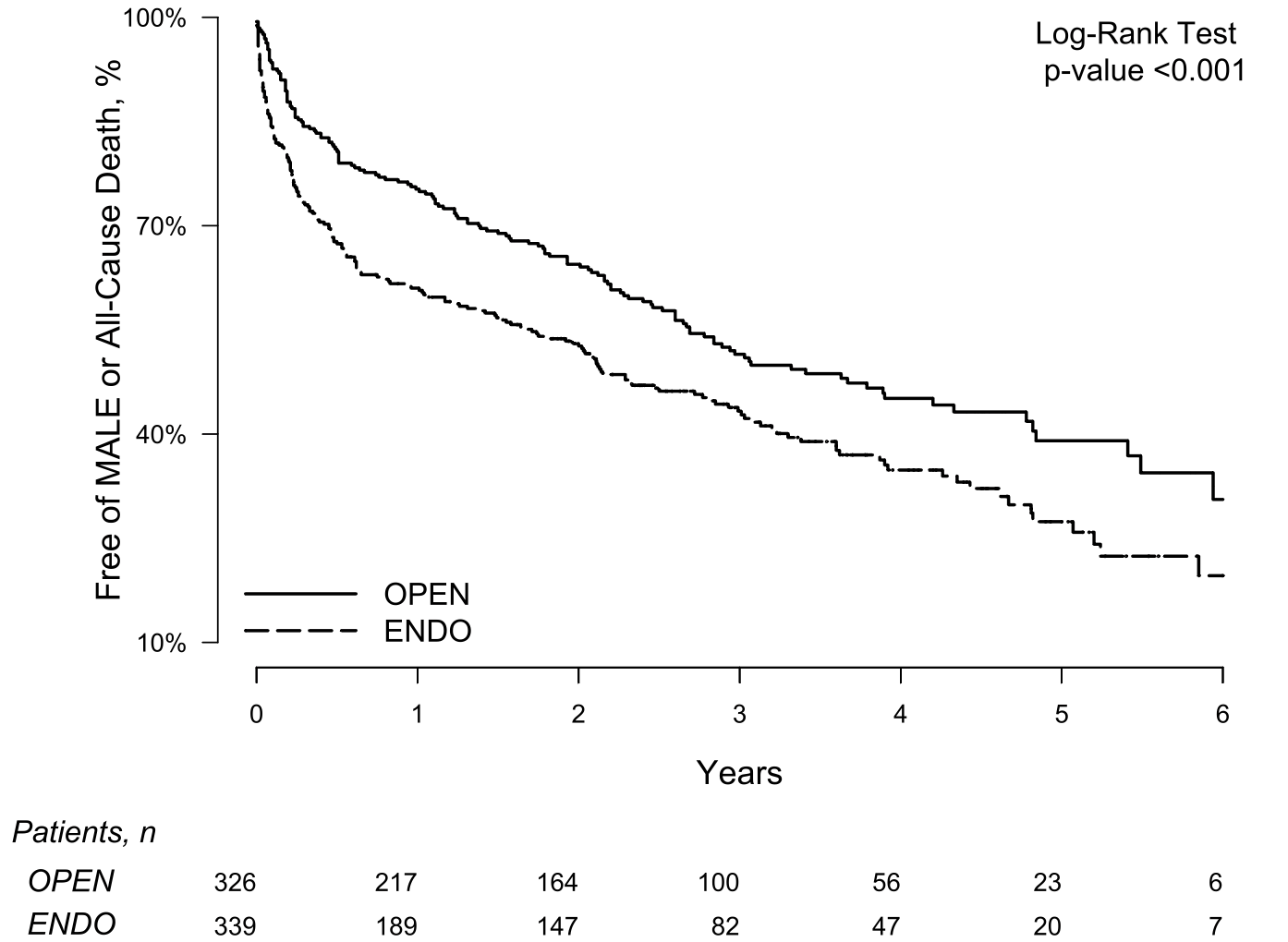
RESULTS: A total of 665 patients were randomized to open tibial bypass(326) or tibial endovascular interventions(339). The primary outcome of MALE or all-cause death at 3 years was significantly lower after open bypass at 48.5% compared to 56.7%(p=0.0006)(Table/Figure). Mortality was similar between groups (35.5% open vs. 35.8% endovascular;p=0.24) whereas MALE events were lower after bypass (23.3% vs. 35.0%;p<0.0001) including major re-interventions (10.9% vs. 20.2%;p=0.0002). Freedom from amputation or all-cause death was similar (43.6% vs. 45.3%;p=0.12) however there was a trend toward lower amputation after bypass (13.5% vs. 19.3%;p=0.053). Perioperative (30-day) death was similar (2.5% vs 2.4%;p=0.93) as was 30-day MACE (5.3% vs 2.7%;p=0.12). Similar results were obtained in the as-treated analyses of the primary and secondary outcomes.
CONCLUSIONS: Among patients with suitable single segment great saphenous vein undergoing infrapopliteal intervention for critical limb ischemia, open bypass surgery had a lower incidence of major adverse limb events or death compared to endovascular intervention and similar amputation free survival. This supports the original conclusion of BEST-CLI favoring bypass surgery and continues to indicate contradictory findings in comparison to BASIL-2.
Table. 3-year outcomes after infrapopliteal open surgical bypass versus endovascular tibial interventions for patients with critical limb ischemia
| All Patients(N=665) | OPEN(N=326) | ENDO(N=339) | ||||||
| N(%) | 3Yr.KM% | N(%) | 3Yr.KM% | N(%) | 3Yr.KM% | HR(95% CI)[OPEN vs ENDO] | p-value | |
| MALE or All-Cause Death | 312(46.9%) | 52.7% | 136(41.7%) | 48.5% | 176(51.9%) | 56.7% | 0.69(0.56,0.85) | 0.0005 |
| All-Cause Death | 204(30.7%) | 35.6% | 99(30.4%) | 35.5% | 105(31.0%) | 35.8% | 0.86(0.68,1.10) | 0.2390 |
| MALE | 171(25.7%) | 29.3% | 62(19.0%) | 22.9% | 109(32.2%) | 35.2% | 0.54(0.40,0.73) | 0.0003 |
| Major Limb Amputation | 93(14.0%) | 16.5% | 37(11.3%) | 13.5% | 56(16.5%) | 19.3% | 0.67(0.45,1.01) | 0.0513 |
| Major Re-intervention | 93(14.0%) | 15.7% | 30(9.2%) | 10.9% | 63(18.6%) | 20.2% | 0.44(0.28,0.68) | 0.0001 |
| Minor Re-intervention | 186(28.0%) | 33.5% | 91(27.9%) | 32.9% | 95(28.0%) | 34.1% | 0.99(0.75,1.32) | 0.9553 |
| Major Amputation or All-Cause Death | 256(38.5%) | 44.4% | 120(36.8%) | 43.6% | 136(40.1%) | 45.3% | 0.84(0.67,1.05) | 0.1216 |
| MACE | 242(36.4%) | 43.3% | 119(36.5%) | 43.2% | 123(36.3%) | 43.4% | 0.94(0.75,1.18) | 0.5700 |
| MI | 70(10.5%) | 13.7% | 39(12.0%) | 15.1% | 31(9.1%) | 12.4% | 1.24(0.80,1.93) | 0.3282 |
| Stroke | 36(5.4%) | 7.7% | 17(5.2%) | 7.2% | 19(5.6%) | 8.3% | 0.75(0.42,1.37) | 0.3547 |