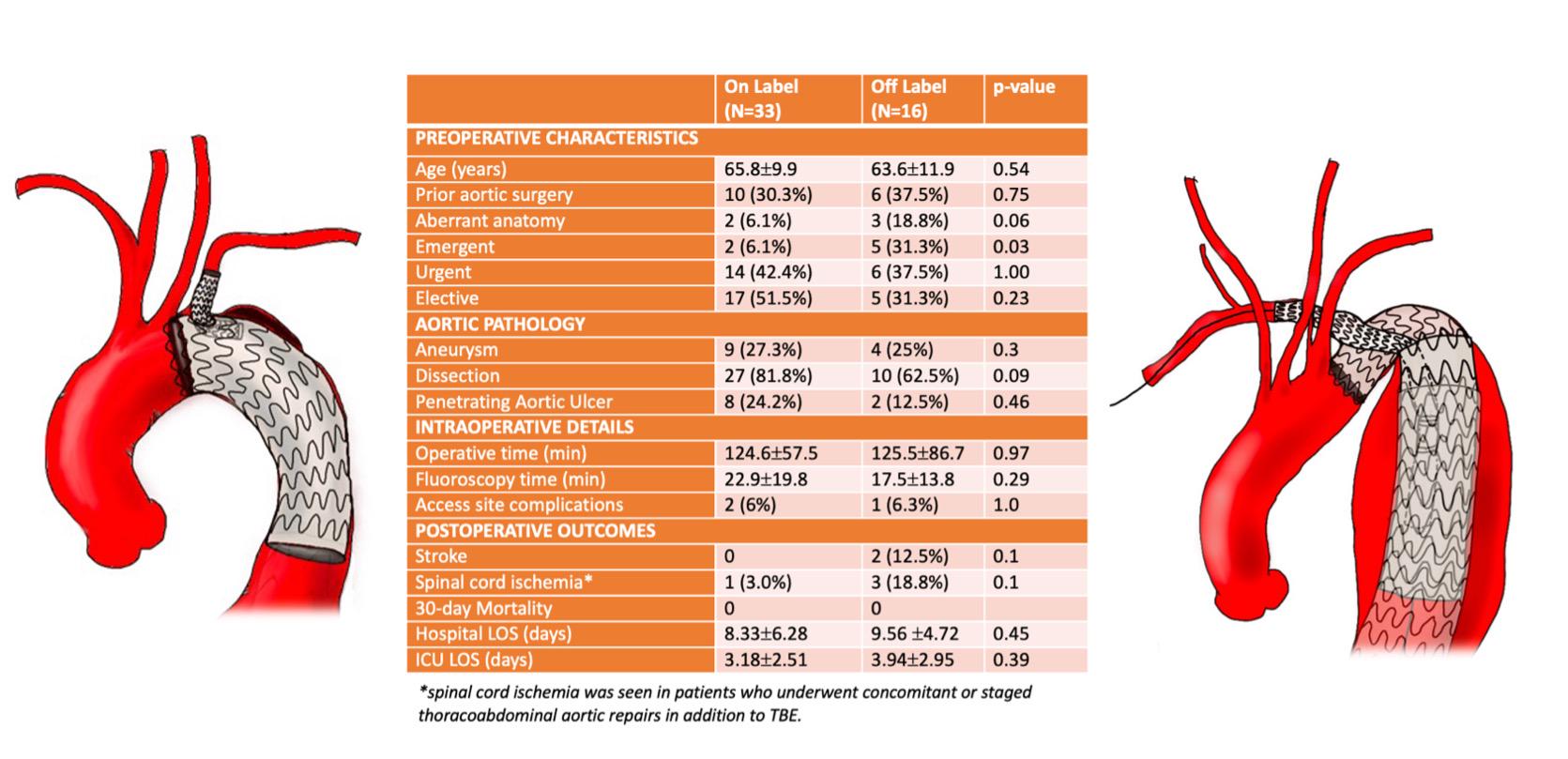
OBJECTIVES: Thoracic Branch Endoprosthesis (TBE) is the first commercially approved off-the-shelf device for left subclavian artery (LSA) incorporation during thoracic endovascular aortic repair (TEVAR). The results of on-label use of TBE within the trials were excellent. However, overall anatomic suitability is limited by the required distance between the carotid and LSA. In urgent settings, this limitation can be overcome by off-label application of TBE. Therefore, we aim to report our early experience of on and off-label application of TBE during zone 2 TEVAR. METHODS:A single-center retrospective review of consecutive patients who underwent zone 2 TEVAR using TBE from 2017 to 2023 was performed. Baseline demographics and initial presentation were reviewed. Intraoperative details, as well as postoperative complications at 30-day including mortality, stroke, spinal cord ischemia were compared between on and off-label groups. Branch patency, type I or III endoleak, and reinterventions during follow-up were compared. RESULTS:Among 49 patients included, 16 (33%) underwent off-label TBE implantation. Off-label TBE was deployed in sandwich periscope configuration consisting of a proximal extension TEVAR device and a longer branch component using Viabahn(W.L. Gore&Associates). Majority (82%) of on-label TBE patients had type B aortic dissections. Emergent repairs were more common in the off-label group (31% vs 6%, P=0.03). Aberrant arch anatomy was more frequent in the off-label group (19% vs 6%, P=0.06). Operative and fluoroscopy times were similar. There was no 30-day mortality. Two off-label TBE patients suffered stroke. Three patients in the off-label group who required concomitant (1) or staged (2) thoracoabdominal aortic repair developed spinal cord ischemia. During follow-up of 17 months, there was 1 patient in each group requiring aortic reintervention for type I endoleak. CONCLUSIONS:
Off-label TBE application using sandwich periscope configuration allows LSA incorporation during zone 2 TEVAR in patients presenting with complex aortic anatomy. While it is a feasible option in urgent, emergent settings, off-label TBE may be associated with higher risk of neurologic complications compared to on-label TBE. Further follow-up is planned to assess the impact of this technique on long-term durability.