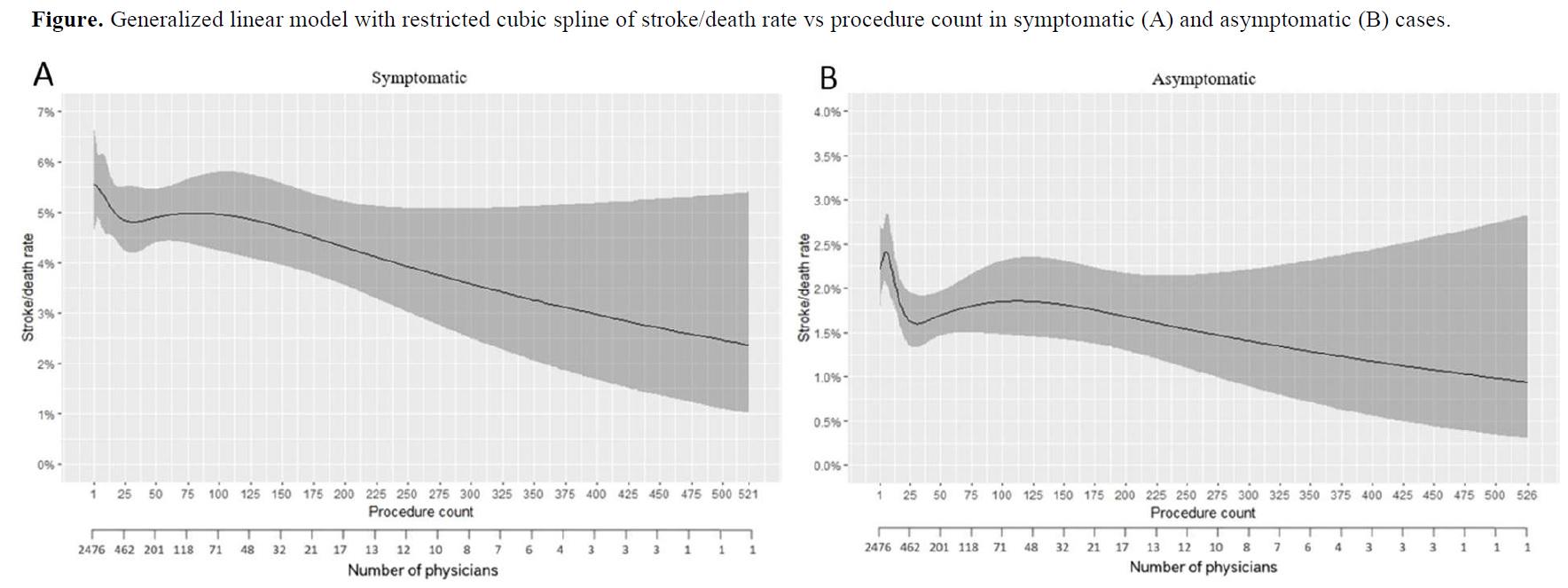
Objective: With potential expansion of the Centers for Medicare and Medicaid Services (CMS) coverage, transfemoral carotid artery stenting (tfCAS) will play a larger role in the management of carotid disease. Existing research on the tfCAS learning curve, primarily conducted over a decade ago, may not adequately define outcomes based on current physician experience. This study evaluates the tfCAS learning curve using VQI data. Methods: We analyzed tfCAS patient data from 2005-2023. Each physician's procedures were chronologically grouped into procedure counts 1-25, 26-50, 51-75, 76-100, 101-125, 126-150, 151-175, 176-200, 201-250, 251-300, 301-350, and 351+. Primary outcome: stroke/death rate; secondary outcomes: stroke/death/MI, 30-day mortality, stroke/TIA, access site complications. The relationship between outcomes and procedure counts as categorical variable was analyzed using the Cochran Armitage test and as a continuous variable using a generalized linear model with restricted cubic splines. Results: We analyzed 43,147 procedures by 2,476 physicians. In symptomatic patients, there was a decreasing trend in rates of stroke/death (1-25 to 351+: 5.2% to 1.7%), stroke/death/MI (5.8% to 1.7%), 30-day mortality (4.6% to 2.8%), stroke/TIA (5.0% to 1.1%), and access site complications (4.1% to 1.1%) as physician experience increased (all p-values<0.05). The stroke/death rate did not drop below 4% until after 240 procedures (Figure A). Similarly, in asymptomatic patients, there were decreasing trends in rates of stroke/death (2.1% to 1.6%), stroke/death/MI (2.6% to 1.6%), 30-day mortality (1.7% to 0.4%), and stroke/TIA (2.8% to 1.6%) with increasing physician experience (all p-values<0.05). Here, the stroke/death rate remained above 2% until 15 procedures (Figure B). We caution that initial cases might not represent physicians’ true first procedures since some may not have recorded them into the VQI database, underestimating the true impact of experience on post-operative outcomes. Conclusions: Adverse postoperative events after tfCAS decreased with increasing physician experience, showing a persistent lengthy learning curve consistent with previous reports. By expanding the CMS coverage for tfCAS, a significant number of physicians will enter the early stage of the learning curve, likely leading to increased postoperative complications.