Objective: Standard Caudo-Cranial Dissection (SCCD) remains the most common surgical approach worldwide for Carotid Body Tumors (CBT) resection. In 2015 we described our initial experience with the Retrocarotid Dissection (RCD) technique and demonstrated significant decrease in procedural time and hospital stay. We aim to follow up and compare the occurrence of intraoperative complications and postoperative outcomes with the use of RCD against SCCD in our institution.
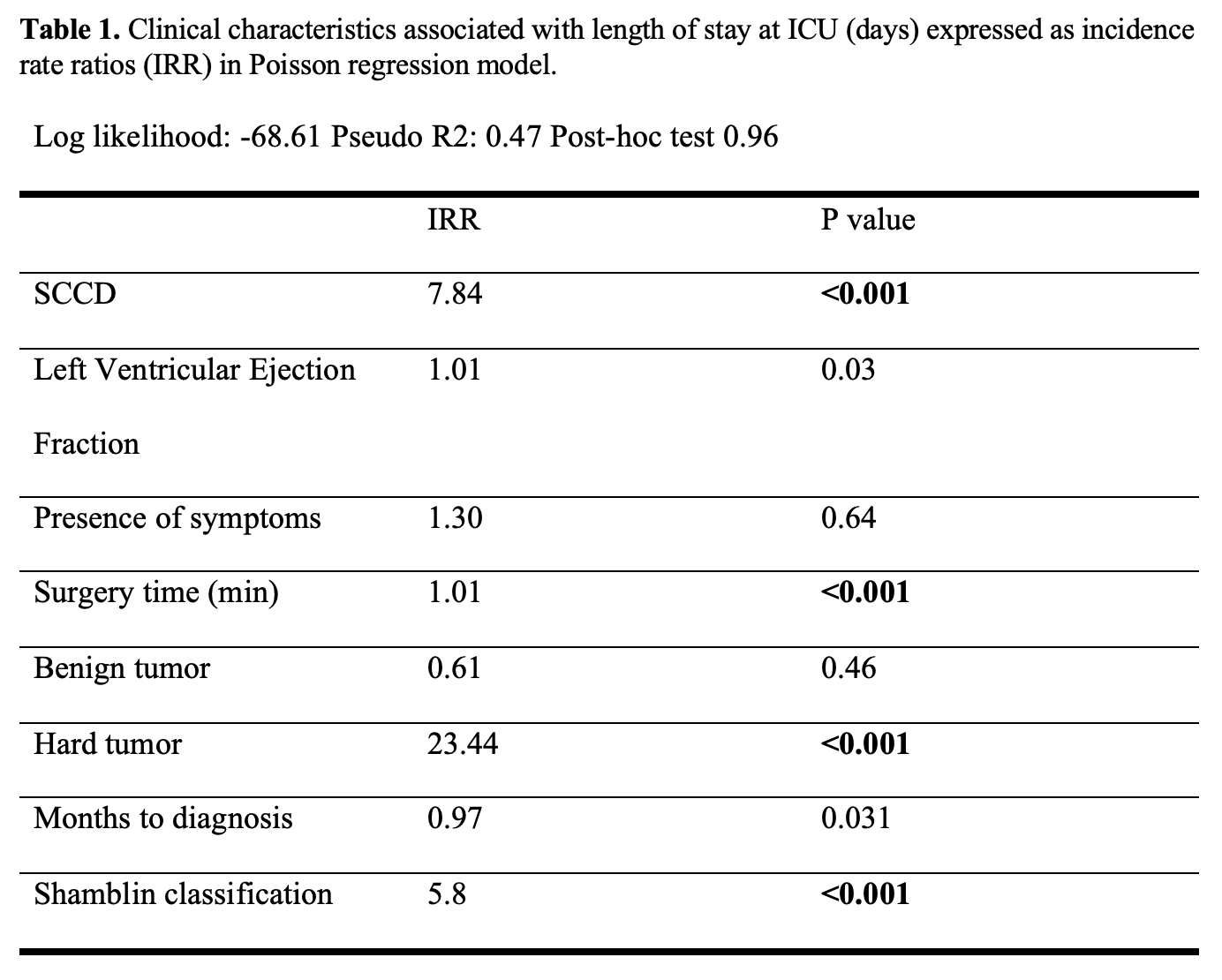
Methods: An observational, retrospective, case-control study in which we analyzed the entirely of the CBT resections that have been performed from 1986 to 2022. Patients were divided by surgical technique (SCCD Vs. RCD) in order to compare both groups. Parametric and non-parametric tests were used accordingly. Finally, a Poisson regression model was performed. Statistical analysis was performed on Stata 17.
Results: A total of 181 surgical procedures were included, mean age was 56.12 years (±13.63) and 168 (93%) were performed in women. Regarding demographics and comorbidities, both groups were equal. Mean medial-lateral diameter was larger in the RCD group (2.85 cm ±1.57 vs. 1.93 cm ±1.85; p=0.001) and pre-surgical embolization was more frequently performed in the SCCD group (27.5% vs. 7%; p< 0.001). A total of 40 (22.09%) resections were performed using SCCD technique, 31 (79.4%) of these CBTs were classified as Shamblin II-III. In contrast, in 140 (77.91%) procedures the RCD technique was used, out of the later, 105 (75%) CBTs were reported as a Shamblin II-III. Mean surgical time in the RCD group was lower (197.31 min ± 70.50 vs. 232 min ± 98.34; p=0.007) and a LOS above the median was more commonly reported in the SCCD group (67.5% vs. 36.87%; p<0.001). Median Length of Stay (LOS) in our series was 4 days. In the Poisson Regression model, SCCD was found to have a greater IRR for days in Intensive Care Unit (Table 1).
Conclusions: The RCD confirms to be a safer option when considering surgical treatment of CBTs in comparison to the SCCD, with a sustained significant decrease in surgical time and overall hospital stay. Additionally, SCDD was associated with longer stay at ICU.