OBJECTIVES: Chronic kidney disease (CKD) and end-stage renal disease (ESRD) are traditionally associated with worse outcomes after procedures for symptomatic and asymptomatic carotid artery stenosis (ACAS). While existing literature focuses on symptomatic carotid artery stenosis, this paper aims to determine whether CKD patients still benefit from carotid revascularization if they are asymptomatic.
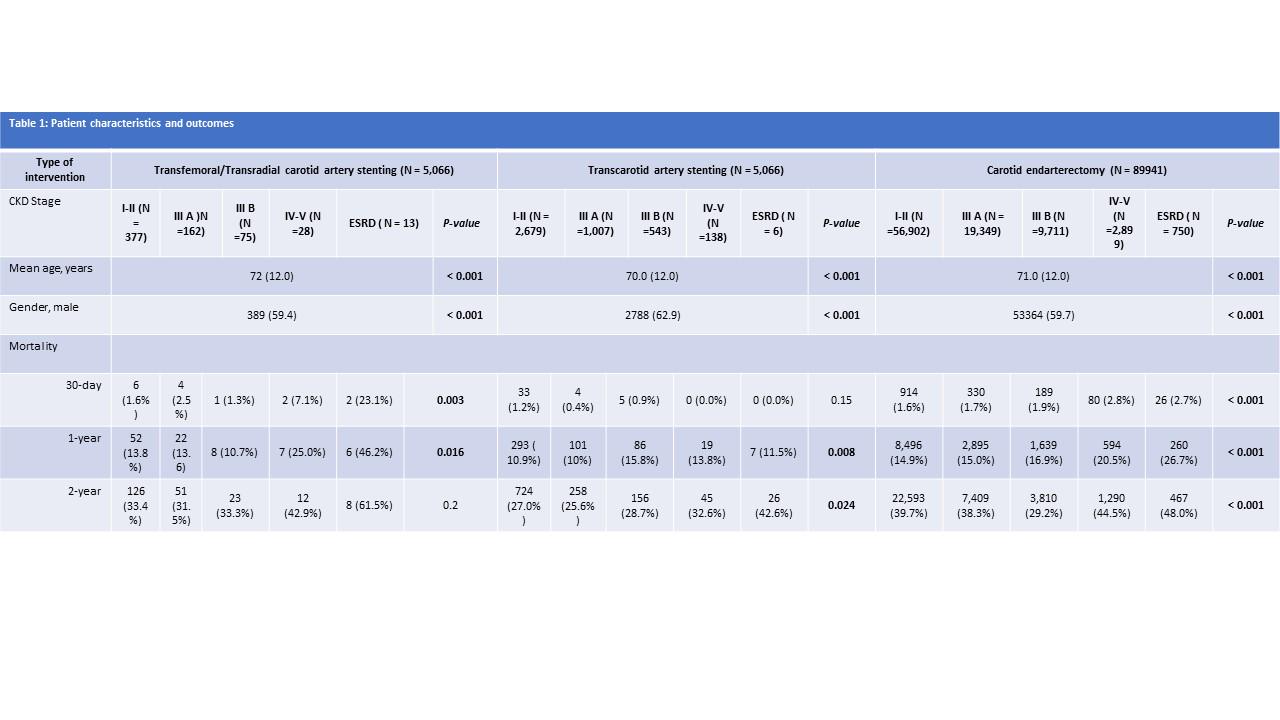
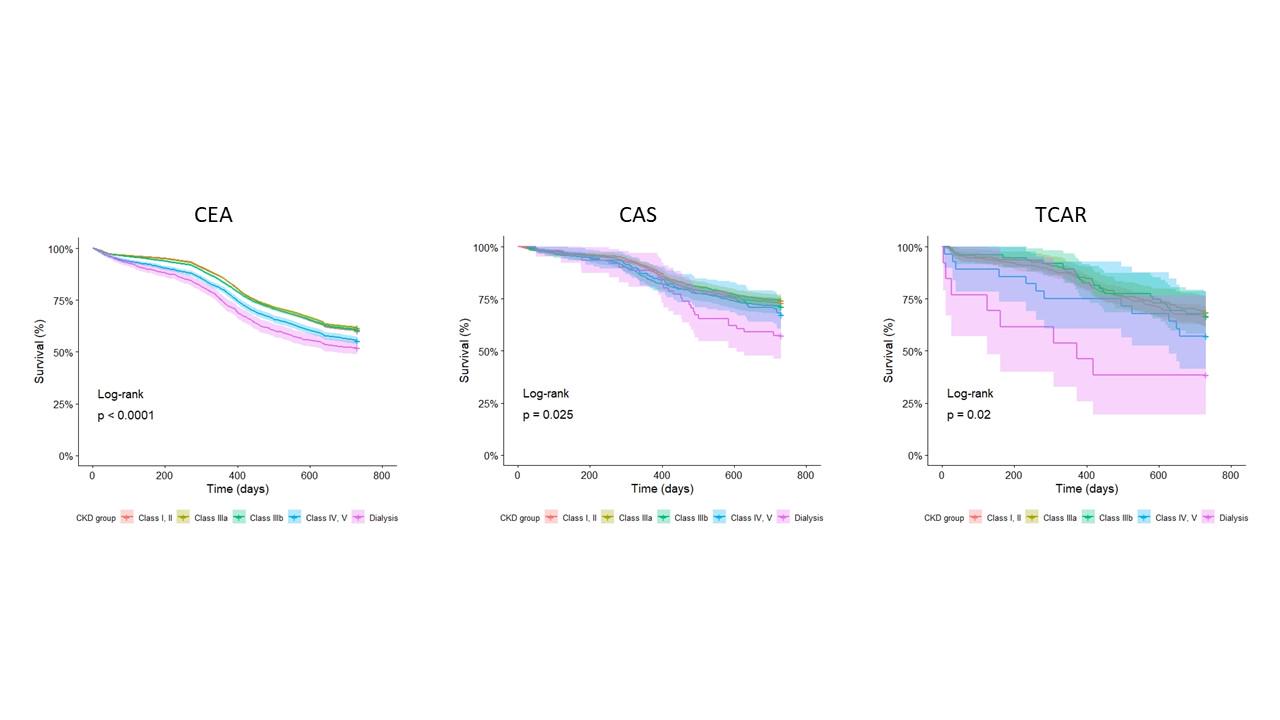
METHODS: Asymptomatic patients in the Vascular Quality Initiative (VQI) registry from January 2003 to September 2020 undergoing elective carotid endarterectomy (CEA), transfemoral/radial carotid artery stenting (CAS), and transcarotid artery revascularization (TCAR) with preoperative renal function data were included. Patients were stratified by renal function as follows: Group 1: normal/mild (CKD stage 1-2), Group 2: moderate (CKD stage 3a), Group 3: moderate-severe (CKD stage 3b), Group 4: severe (CKD stage 4-5), and Group 5: dialysis. Primary outcomes were 1- and 2-year mortality. Kaplan-Meier estimates of 1- and 2- year survival and cox regression models for 1- and 2-year mortality were performed.
RESULTS: Out of 99,973 CKD patients who underwent carotid interventions for ACAS, 90% underwent CEA, 5% CAS, and 5% TCAR. Table 1 depicts demographics and outcomes after each approach. Figure 1 shows Kaplan Meier analysis of 2-year of survival, with worse outcomes for patients with GFR <30 after any intervention. On cox regression analysis, compared to CKD Group 1, CKD groups 4 and 5 (HR 1.19 and 1.37, respectively, p<0.001), had worse 2-year mortality after CEA. After CAS and TCAR, only dialysis (HR 1.69 and 2.95 respectively p <0.05) was predictive of worse 2-year mortality.
CONCLUSIONS: CKD severity is an important predictor of 2-year mortality for ACAS interventions regardless of the treatment approach. Given the high 1- and 2- year mortality, patients with CKD stage 4 and 5 and dialysis may not be good candidates for asymptomatic carotid interventions. Decision to operate on CKD stage 3 patients should be individualized.