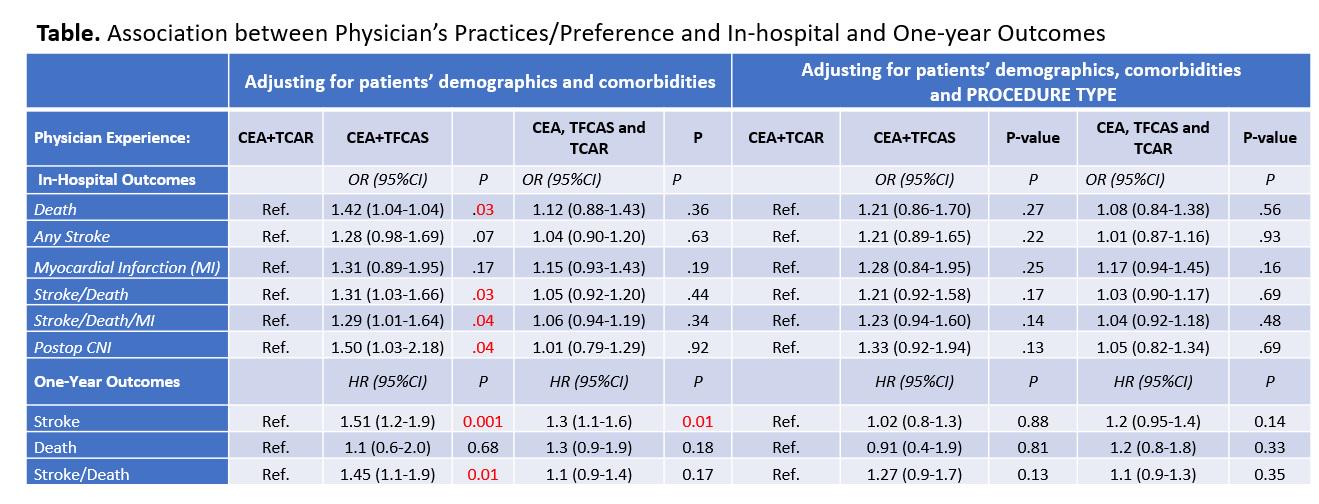
OBJECTIVES: Options for carotid revascularization include endarterectomy (CEA), transfemoral stenting (TFCAS) or Transcarotid artery revascularization (TCAR). However, the choice of these procedures is at the discretion of treating physicians. The aim of this study is to explore the overall outcomes of carotid revascularization based on physicians’ preferences, who are facile with at least 2 of the three available procedures.METHODS: Individual physicians participating in both the CAS and CEA Vascular Quality Initiative registries (2016-2022) were categorized as performing CEA+TCAR; CEA+TFCAS; or all 3 procedures. Physicians performing CEA only or TCAR/TFCAS only were excluded. In-hospital and 1-year outcomes were compared between the 3 groups using univariable and multivariable analysis. RESULTS:A total of 104925 carotid procedures performed by 1433 physicians were included. Almost half of the included cases (49.7%) were done by physicians who usually perform all 3 procedures,39% by those practicing CEA+TCAR and 11.2% by those practicing only CEA and TFCAS. CEA was the most common procedure performed by the 3 groups of physicians. Patients undergoing revascularization by CEA+TFCAS physicians were younger, more likely to be symptomatic, had less medical comorbidities and lower use of statins and P2Y12 inhibitors compared with patients in the CEA+TCAR and CEA+TFCAS+TCAR groups. Physicians performing CEA+TFCAS had higher overall stroke/death rates(2.2%) compared with those performing CEA+TCAR (1.4%) or those performing all 3 procedures(1.6%,P<.001). They also had higher rates of cranial nerve injuries (3.1% vs.1.9%vs.1.9%,P<.001). On adjusted analysis, procedures performed by CEA+TFCAS physicians had significantly higher odds of in-hospital stroke/death compared with those in the CEA+TCAR group [OR(95%CI),1.31(1.03-1.66;P=.03]. They also had higher stroke/death hazard at 1-year [HR(95%CI),1.45 (1.1-1.9),P=.01]. No significant differences in perioperative and 1-year stroke/death outcomes were observed between CEA+TCAR performers versus (CEA+TCAR+TFCAS) performers(Table).When adjusting for the type of carotid revascularization technique, there was no longer a difference in outcomes based on surgeon’s experience, indicating that differences in outcomes were procedure-specific and attributable to the inferior outcomes associated with TFCAS compared to CEA and TCAR.
CONCLUSIONS: Physicians' preference has a bearing on their overall stroke/death rates. Careful patient and procedure selection are the cornerstone to improve carotid revascularization outcomes. Surgeons who perform CEA+TCAR have lower reported stroke/death rates.