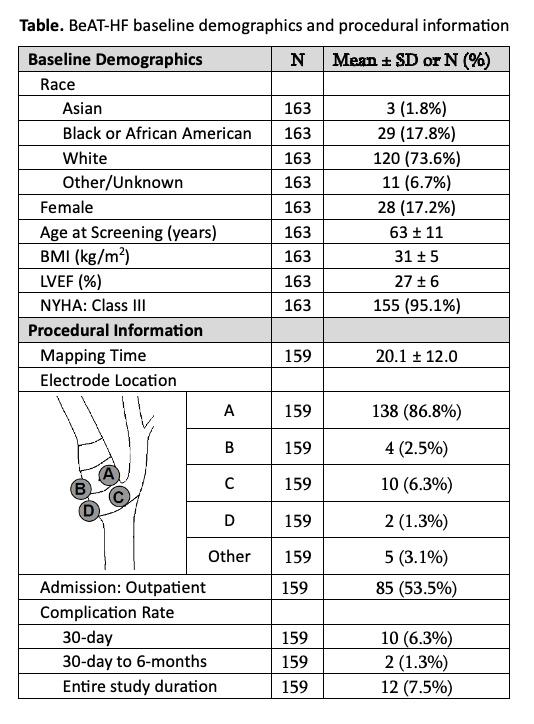
OBJECTIVE: Electrical stimulation of the carotid baroreceptors, known as Baroreflex Activation Therapy (BAT), has been postulated to be of benefit for the treatment of patients with heart failure and/or resistant hypertension. Vascular surgeons, due to their knowledge of carotid and cranial nerve anatomy, have been the predominant implanters. Herein we report the intraoperative surgical experience and long-term safety observed in the recently concluded BAT for Heart Failure (BeAT-HF) pivotal trial.METHODS: Patients with reduced ejection fraction NYHA Class II/III heart failure were randomized 1:1 to receive BAT plus guideline directed medical therapy (GDMT) or GDMT alone. The BAT implant procedure involved mapping an electrode on the surface of the carotid sinus and surgically implanting the electrode in a location that produced the maximum baroreflex response. Procedural information as well as safety and efficacy data were collected as part of the trial.RESULTS: A total of 159 patients were implanted with the BAT system. Average carotid sinus mapping time was 20.1 ± 12.0 minutes, which showed improvement with experience. Surgical experience also documented that the majority of electrodes (87%) were placed at the anteromedial aspect of the internal carotid artery (Table). Five major adverse neurologic and cardiovascular events (MANCE) occurred within 30-days after implantation: two infections that required explant, neck pain that required lead repositioning, a stroke, and a decompensation of heart failure that required hospitalization, accounting for a 96.9% MANCE free rate. The system- or procedure-related complication rate within 30-days and 30-days to 6-months after implant was 6.3% and 1.3%, respectively. Throughout 41.9 ± 15.4 [1.2-72.1] months of implant follow-up in BeAT-HF, a system- or procedure-related complication occurred in 12 patients, accounting for a 92.5% complication-free rate. Overall, 12-24-month therapeutic benefit from BAT was consistent with previously reported efficacy through 6 months: there was a durable clinically meaningful improvement in quality of life, 6-minute hall walk distance, and NYHA Class.CONCLUSIONS: BAT appears to be an effective therapy for patients with NYHA Class II/III heart failure. Despite the significant risk profile of this patient population, surgical implantation of the BAT system was attended by low perioperative and long-term complications.