OBJECTIVE
Vascular integrated residency and vascular surgery fellowship training paradigms offer two unique pathways to independent vascular surgery practice. Although operative requirements are equivalent in each, it is unknown whether operative competency achieved is comparable between paradigms. We sought to examine operative performance and autonomy achieved between vascular integrated residents (VIR) and fellows (VSF) in their graduating year.
METHODS
Operative assessments were collected between 2018-2022 from a national cohort of vascular surgery training programs using the Society for Improving Medical Professional Learning (SIMPL) application. Summary statistics including the number of assessments and participants stratified by training paradigm were presented. Generalized linear mixed models were conducted to examine the differences in the assessments of autonomy and performance between VIR and VSF in their graduating year, controlling for case complexity and procedure types (open or endovascular). To account for the statistical dependency within the nested data, the random effects of trainee, faculty, program and procedure were included. Analyses were conducted for faculty and trainee assessments, separately. Data were analyzed using R software.
RESULTS
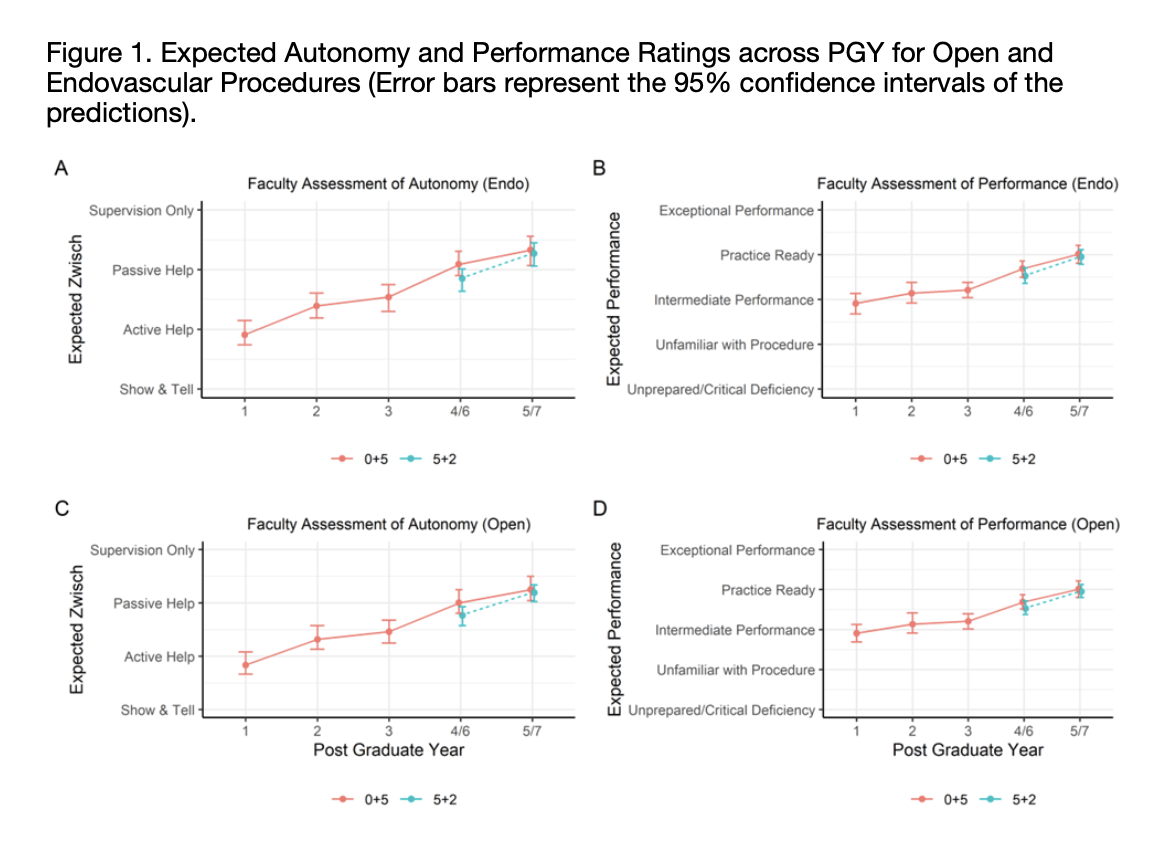
4,927 assessments (n=2,232 assessments by faculty; 2,695 assessments by trainees) were collected from 106 trainees and 94 faculty from 25 programs (n=12 residency, 13 fellowship). There were no differences in faculty or trainee assessments of operative performance (faculty: β = 0.063, P = 0.564; trainee: β = -0.145, P = 0.191) or autonomy (faculty: β = 0.062, P = 0.607; trainee: β = 0.025, P = 0.834) between VIR and VSF at completion of training, even when corrected for case complexity and procedure type. Using the model, the predicted performance and autonomy ratings for VIR and VSF were estimated across PGY for open and endovascular procedures, respectively (Figure 1). There were also no differences when comparing open vs endovascular procedures between VIR and VSF trainees.
CONCLUSIONS
Upon completion of training, operative performance and autonomy are comparable between VIR and VSF trainees for endovascular and open procedures as assessed by both faculty and trainees. Despite inherent differences in the training paradigms, equivalent competency and autonomy are achieved by graduation ensuring preparedness for independent practice.