Introduction: Conversations regarding trainee compensation is infrequently discussed; its importance as a consideration for trainees in ranking programs is unknown. However, for an evolving surgical workforce facing record inflation and significant educational debt, compensation during the 5-7 years of vascular surgery training warrants investigation. The purpose of this study was to examine vascular surgery trainee compensation in the context of geographic variation in cost-of-living (COL).
Methods: Salary data for 118 vascular fellowships (VF) and 73 integrated vascular residency (IVR) programs were obtained via program websites. Salary in the first year of vascular training (PGY1 for IVR; PGY6 for VF) were used to perform descriptive analysis of compensation. Salary data were linked to publicly available COL indices for the respective locations, allowing for calculation of an appropriate “expected” salary based on COL for each program locale.
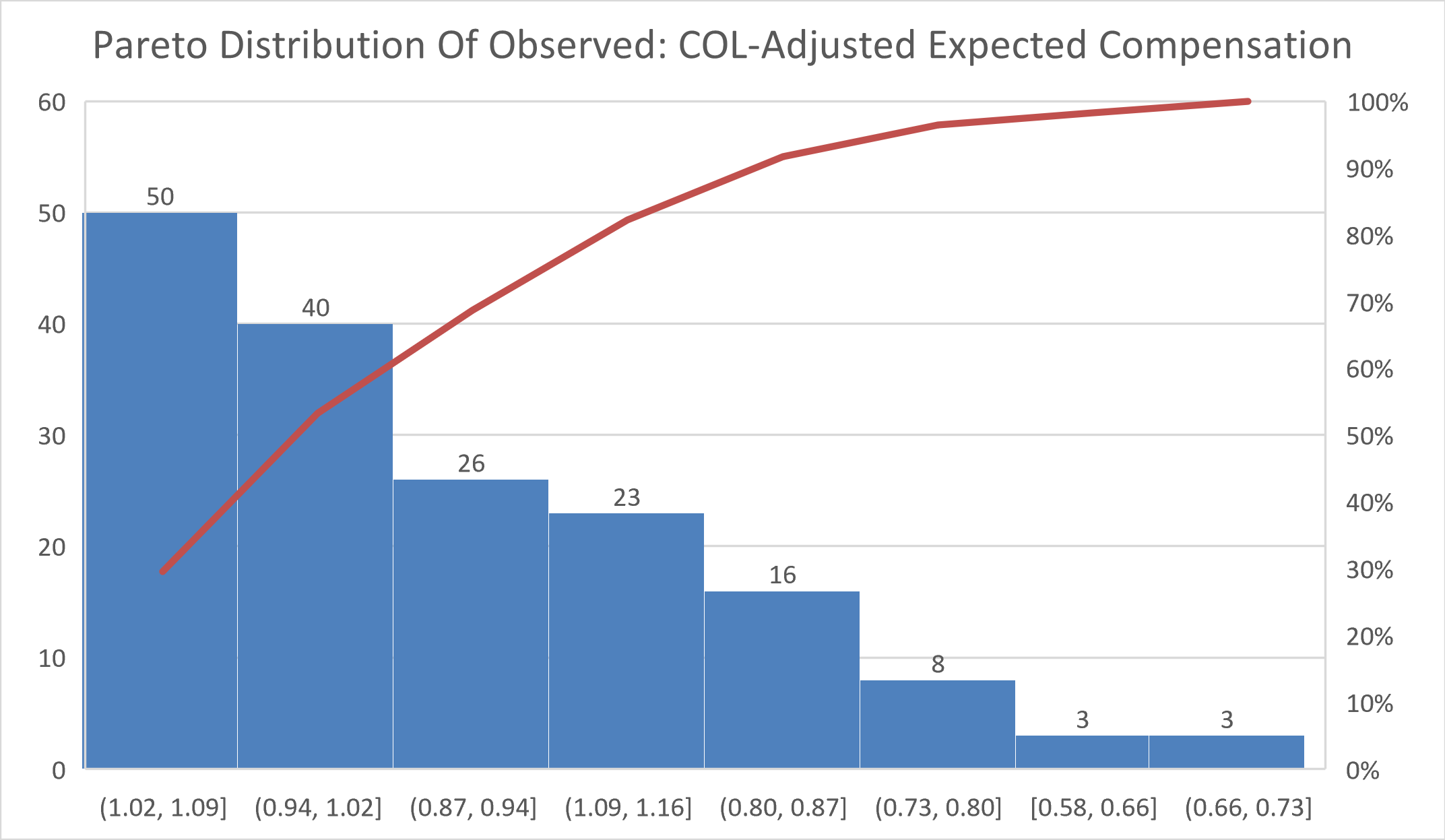
Results: Median salaries for IVR PGY1 and VF PGY6 years were $61,794 (range $53,355-$75,000) and $73,384 (range $62,441-$88,189) respectively. 113 programs (59.2%) offer compensation that is within 5% of the COL-adjusted expected salary. 14 programs (7%) compensate trainees at below 80% of COL-adjusted expected compensation (Figure 1). 6 programs (3.1%) compensate trainees at less than 66% of COL-adjusted expected salary.
Conclusion: While there is only modest variation in actual salary at the PGY1 and PGY 6 levels for IVR and VF programs, significant geographic variation in the cost of living may impact trainees’ financial well-being. Even though compensation is greater in areas with higher COL, vascular surgery trainees in these high-cost locales remain disproportionately affected. These findings have obvious implications for trainees, program directors, and institutional graduate medical education policy.images/