Objective: Venous thoracic outlet syndrome (vTOS) is caused by compression of the subclavian vein at the costoclavicular space, which may lead to vein thrombosis. Current treatment includes thoracic outlet decompression with or without venolysis. However, given its relative low prevalence, the existing literature is limited. Here, we report our single institution experience in the treatment of vTOS.
Methods: We performed a retrospective review of all patients who underwent rib resection for vTOS at our institution from 2007 to 2022. Demographic, procedural details, perioperative and long-term outcomes were reviewed.
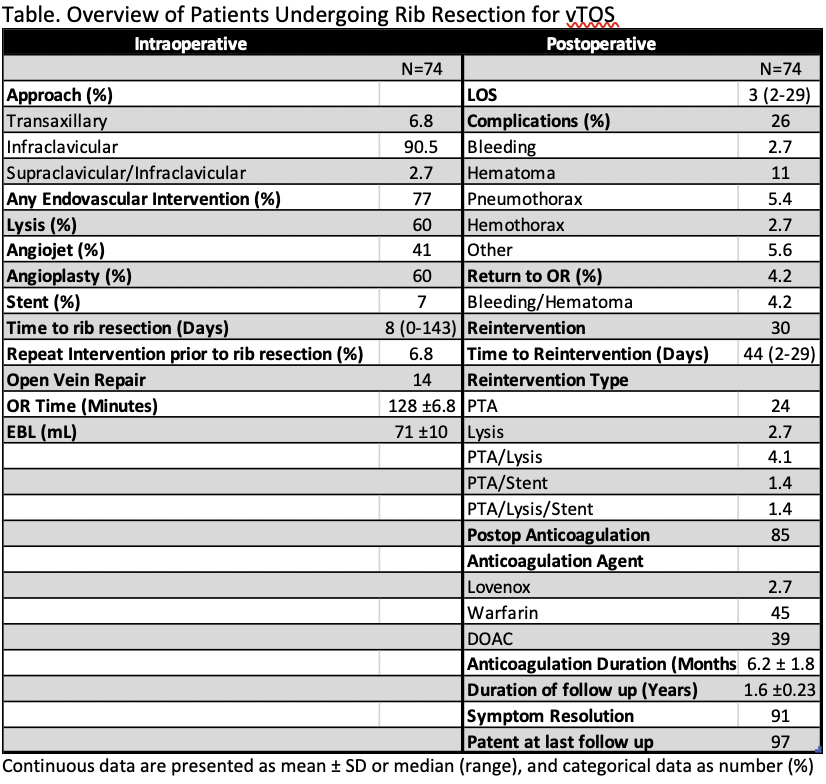
Results: A total of 74 patients were identified. The mean age was 36y. 51% were female. Swelling was the most common symptom (92%), followed by pain (6.8%). 80% of patients had associated DVT, with 95% of these patients starting anticoagulation preoperatively. 91% of patients underwent rib resection via infraclavicular approach, 2% via paraclavicular approach (due to neurogenic component), and 7% via transaxillary approach (4/5 cases prior to 2009) (Table). 77% of patients had endovascular intervention prior or at the time of the rib resection, with 60% of all patients having catheter-directed-thrombolysis, 41% rheolytic thrombectomy, 60% angioplasty, and 7% stenting. Median time from endovascular intervention to rib resection was 8 days, 43% occurring during same admission. Average operative time was 128 minutes. Median postoperative stay was 3 days (2-29). 26% of patients had complications, including 4% operative intervention for bleeding. There were no brachial plexus injuries. 85% of patients were discharged on anticoagulation. Median duration of anticoagulation was approximately 6 months. 30% required reintervention, most commonly angioplasty (24%). The median time to reintervention was 44 days. At last follow-up (1.6y), 97% of subclavian veins were patent, and 91% of patients were symptom-free.
Conclusion: Over the last decade we have transitioned to an infraclavicular approach for isolated vTOS, with low perioperative morbidity and good patency rates. These results support the adoption of the infraclavicular approach with adjunct endovascular techniques as a safe and efficacious treatment of vTOS.