OBJECTIVES: Due to the rarity of median arcuate ligament syndrome (MALS), surgical approaches to median arcuate ligament release (MALR) have been difficult to study for efficacy and safety. This series aimed to review robot-assisted laparoscopic MALR from a tertiary care center
METHODS: Retrospective chart review was performed on all patients over the age 18 who underwent robot-assisted laparoscopic MALR between March 2015 and June 2023 at our institution. Data was collected from providers’ notes before and after MALR. Long-term outcomes were determined by chart review of the medical record. Data analysis included basic descriptive statistics and Fisher’s exact test.
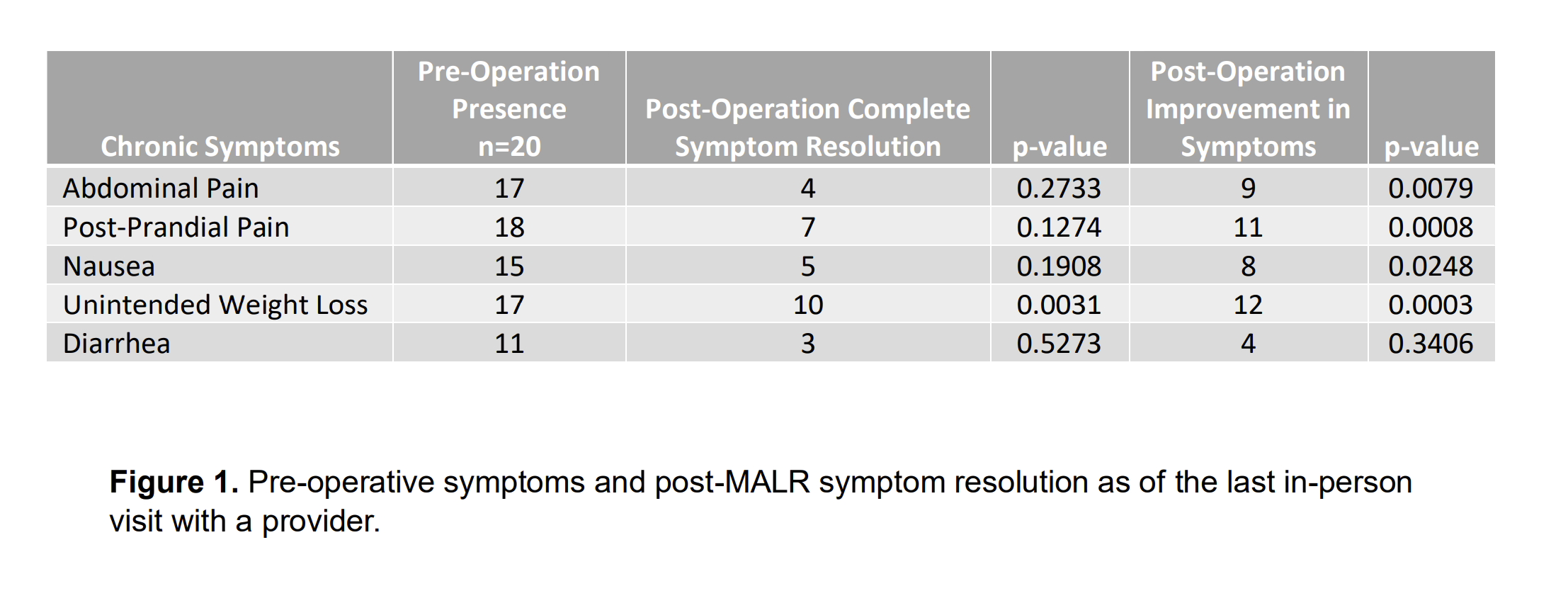
RESULTS: 20 patients were included in this series. The mean age of patients at the time of surgery was 41.65 (±16.02) and 16 (80%) of the patients were female. Concomitant gastrointestinal illnesses included Crohn’s/IBS (40%) and GERD (35%). DSM-5 psychiatric illnesses were diagnosed in 13 (65%) patients. Duplex ultrasonography performed on all patients pre-operatively indicated a mean pre-operative max celiac peak systolic velocity (PSV) of 376.39 (±109.66) cm/s. Duplex was obtained on 60% of patients post-operatively, demonstrating a max PSV of 326.52 (±107.32) cm/s. Additional duplex data was gathered more than three months postoperatively in 45% of patients demonstrating a mean PSV of 251.25 (±77.71) cm/s. The most frequently encountered pre-operative chronic symptom was post-prandial pain (90%). Post-operatively, as of the last in-person provider note, 10 patients experienced complete resolution of unintended weight loss (p=0.0031), and significant improvement in chronic MALS symptoms including abdominal pain, post-prandial pain, and nausea (figure 1). The median follow-up time was 1.63 (0.97 - 2.69) years. Operative characteristics include mean operative time of 197.11 (±37.53) minutes, median estimated blood loss of 20 (8.75 - 25.00) mL, and a median of 2 (1-3) days hospital stay post-operatively. 2 patients experienced a return to the OR.
CONCLUSIONS: Our single institution experience offers evidence that robot-assisted laparoscopic MALR can be a safe, viable option for long-term relief of MALS symptoms. Further research is needed to validate our results. To better evaluate the efficacy and safety of this approach, prospective, randomized studies comparing robot-assisted MALR to other methods are needed.