OBJECTIVES: Endovascular aneurysm repair (EVAR) has gained favor over Open repair for non-emergent abdominal aortic aneurysms (AAA). This study characterizes the trends and outcomes of EVAR and Open repair for elective AAA over 20 years in the VA Health Care System.
METHODS: All patients who underwent elective EVAR or Open AAA repair in the VA Surgical Quality Improvement Program (VASQIP) database between 1/1/2002 - 12/31/2019 were identified using CPT and ICD-9/10 codes. 30-day mortality and morbidities including returning to operating room, acute renal failure, and pulmonary embolism (PE) were compared. Categorical variables were analyzed using Chi-squared test whereas continuous variables using Wilcoxon rank-sum test.
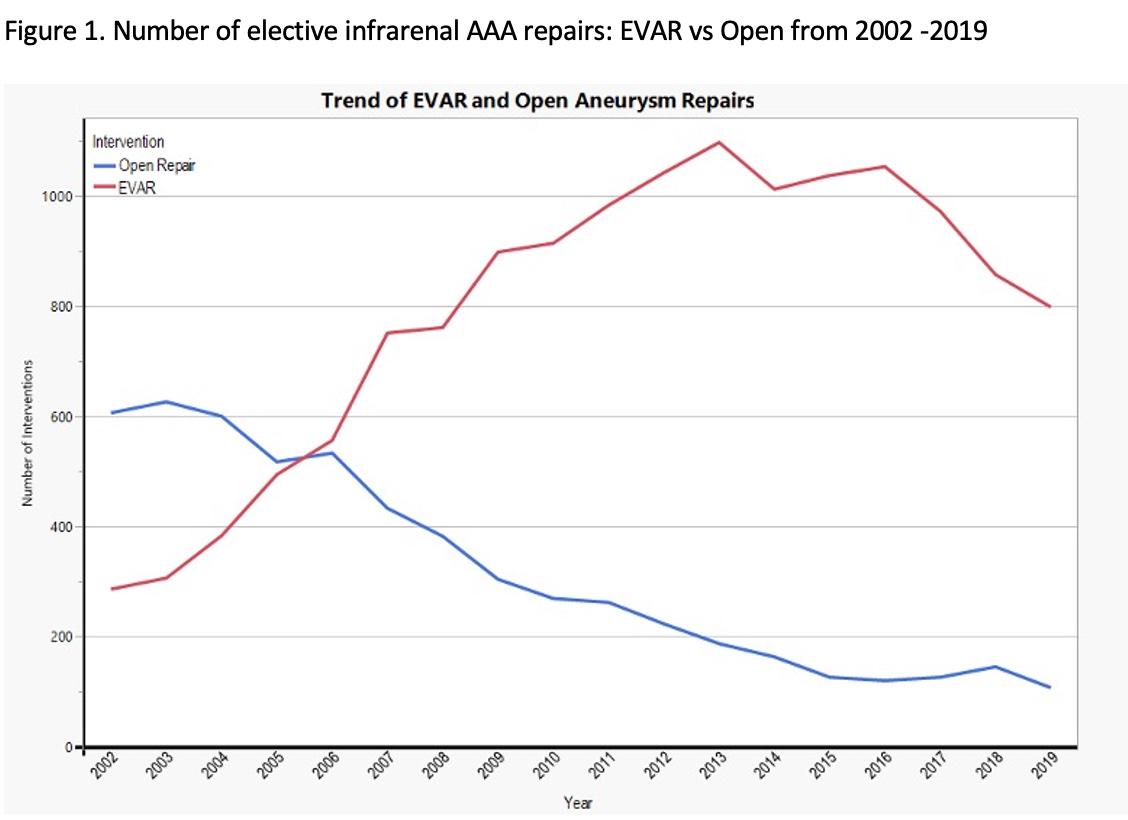
RESULTS: A total of 20,163 patients with a mean age 70.5±7.9 years were included. Approximately half were smokers. EVAR was performed on 70.7% of the patients and Open repair on 29.3%. The number of Open repairs steadily declined while the number of EVARs performed increased and surpassed that of Open repairs in 2006. However, the volume of both Open repair and EVAR started decline in 2011 (Figure1). Open repair was associated with higher rate of 30-day mortality compared to EVAR, but the mortality was significantly lower for both procedures after 2010 compared to prior to 2010 (4.3% vs 3.1% for Open and 1.6% vs 0.8% for EVAR, p<0.05). Overall, Open repair was associated higher rates of returning to the OR (9.6% vs 4.6%, p<0.001), post-op renal failure (2.8% vs 0.5%, p<0.001), and post-op PEs (0.6% vs 0.1%, p<0.001).
CONCLUSIONS: Perioperative outcomes of elective EVAR and Open repair for infrarenal AAA in the VA Health Care System are comparable to the OVER Trial and improved over time. However, there is a trend of steady decline in the number of aneurysm repairs in the last decade. Further studies are warranted to explore characteristics modulating mortality and morbidities.