Objective: While complex abdominal aortic aneurysms (AAAs) have traditionally been repaired through open operations (cOARs), there has been a significant rise in endovascular repairs (cEVARs). We evaluated long-term outcomes among patients who were discharged alive after their index hospitalization, and how these outcomes varied by the presence of a postoperative complication.
Methods: We identified all elective complex AAA repairs in the 2014-2019 VQI-VISION registry, which couples the granularity of the Vascular Quality Initiative registry with Medicare long-term outcomes. Short-term outcomes included: perioperative mortality, complications, and failure-to-rescue. After dichotomizing patients who survived the index hospitalization into those that did not and those that did experience a postoperative complication, we evaluated two long-term outcomes: 3-year all-cause mortality and 3-year reinterventions. Multivariable logistic regressions and cox-proportional hazards models evaluated short-term and long-term outcomes, respectively.
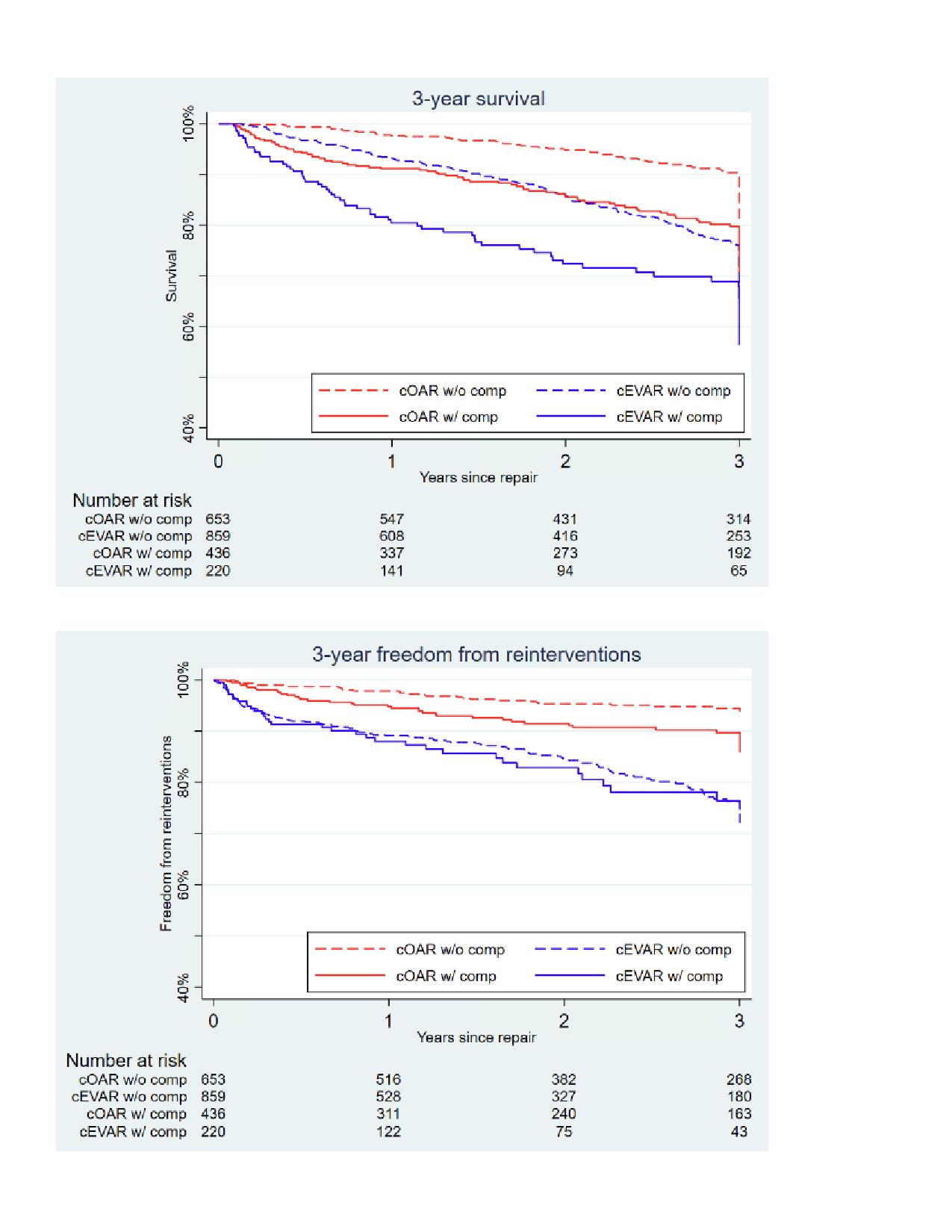
Results: We identified 2271 patients (50% cOARs, 50% cEVARs). Relative to cOARs, cEVARs had lower rates of perioperative mortality (4.1% vs 5.0%, aOR 0.61 [95%-CI 0.40-0.95], P=.03) and complications (23% vs 42%, aOR 0.36 [0.29-0.45], P<.01) but similar rates of FTR (15% vs 10%, aOR 1.33 [0.75-2.37], P=.32). Among 2168 patients (95%) who were discharged alive, 1512 (70%) did not and 656 (30%) did have a postoperative complication. Among the patients discharged alive who did not have a postoperative complication (Figure), cEVARs had higher rates of 3-year all-cause mortality (24% vs 9.6%, aHR 1.92 [1.41-2.61], P<.01) and reinterventions (24% vs 5.6%, aHR 4.36 [2.85-6.67], P<.01). Similarly, among patients discharged alive who did have a postoperative complication (Figure), cEVARs had higher rates of both 3-year all-cause mortality (32% vs 20%, aHR 1.45 [1.01-2.09], P<.05) and reinterventions (24% vs 10%, aHR 2.43 [1.45-4.07], P<.01).
Conclusion: Our findings continue to support the observation that while cEVARs have lower short-term mortality and complications, they have higher 3-year all-cause mortality and reinterventions relative to cOARs, irrespective of the presence of a postoperative complication. Clinical decision making for open versus endovascular repair of complex aneurysms should take long term durability and survival into consideration, and ideally a randomized controlled trial for complex AAA repairs would make an important contribution in the care of these patients.