Objective: Patient travel time to the hospital is a key metric of individual and social disadvantage and its impact on the management and outcomes following intervention for chronic limb-threatening ischemia (CLTI) is likely underestimated. We sought to evaluate the effect of travel time on outcomes in patients undergoing first time lower extremity revascularization at our institution.
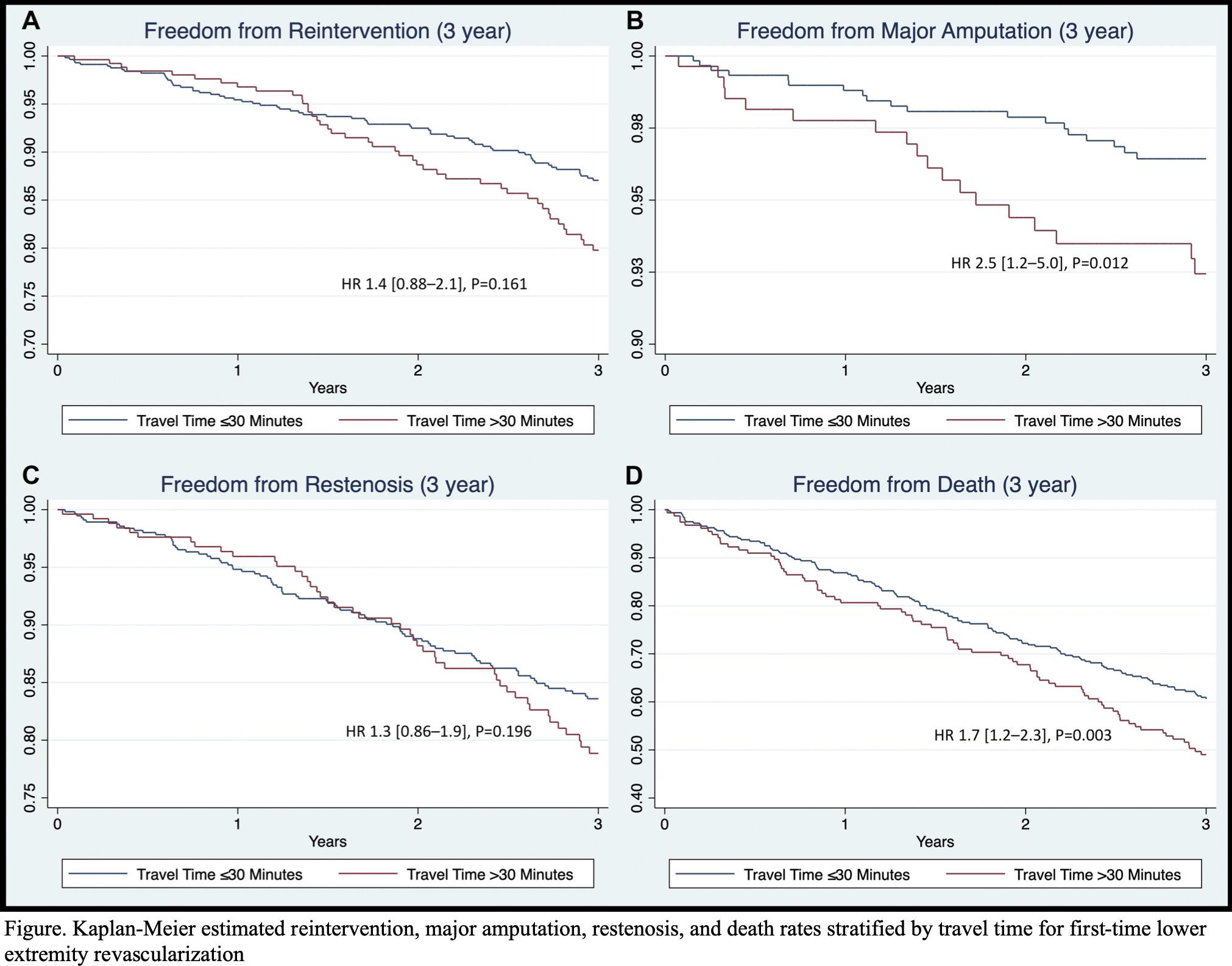
Methods: We retrospectively reviewed all consecutive patients undergoing first-time lower extremity revascularization, both endovascular and open, for CLTI from 2005 to 2014. Patients were stratified into 2 groups based on travel time from home to hospital greater than or less than 30 minutes. Outcomes included reintervention, major amputation, restenosis, primary patency, wound healing, length of stay, length of follow-up and mortality. Kaplan-Meier estimates were used to determine event rates. Logistic and cox regression was used to evaluate for an independent association between travel time and these outcomes.
Results: Of the 1,293 patients were identified, 490 (38%) traveled more than 30 minutes. Patients with longer travel time were younger (70 vs 73 years, P=0.0013), more likely to undergo open revascularization (65% vs 41%, P<0.001), and had slightly lower mean WIFI scores (1.3 vs 1.4, P=0.001). There were similar rates of tissue loss (84% vs 85%, P=0.848) in both groups. Longer travel time was associated with an increase in total hospital length of stay (9.6 vs 8.6 days, P=0.031) and lower total length of post-operative follow-up (2.1 vs 3.0 years, P=0.001). At 3-years, there was no definitive difference in the rate of restenosis (HR 1.3[0.86-1.9, P=0.196) or reintervention (HR 1.4[0.88-2.1, P=0.161), but longer travel time was associated with an increased rate of major amputation (HR 2.5[1.2-5.0], P=0.012), and death (HR 1.7[1.2-2.3], P=0.003) (Figure). Longer travel time was also associated with higher rate of non-healing wounds (HR 1.8[1.1-3.1], P=0.001).
Conclusion: Longer patient travel time was found to be associated with a lower likelihood of limb salvage and survival in patients undergoing first-time lower extremity revascularization for CLTI. Understanding and addressing the barriers to discharge, need for multidisciplinary follow-up, and appropriate post-operative wound care management will be key in improving outcomes at tertiary care regional specialty centers.