Demographics: Loeys-Dietz (LDS) and Vascular Ehlers-Danlos syndromes (vEDS) are genetic aortopathies associated with vascular complications and early death. We present a case of staged thoracoabdominal aortic aneurysm (TAAA) repair in a patient with confirmed genetic mutations for both LDS (SMAD3) and vEDS (COL3A1).
History: A 34-year-old male presented with a 7.0 cm aneurysm of the aortic arch. He previously underwent an ascending aortic repair for a type A aortic dissection four years prior. He reported easy bruising and a family history of abdominal aortic aneurysms. Given the need for an extensive repair, a staged repair was planned.
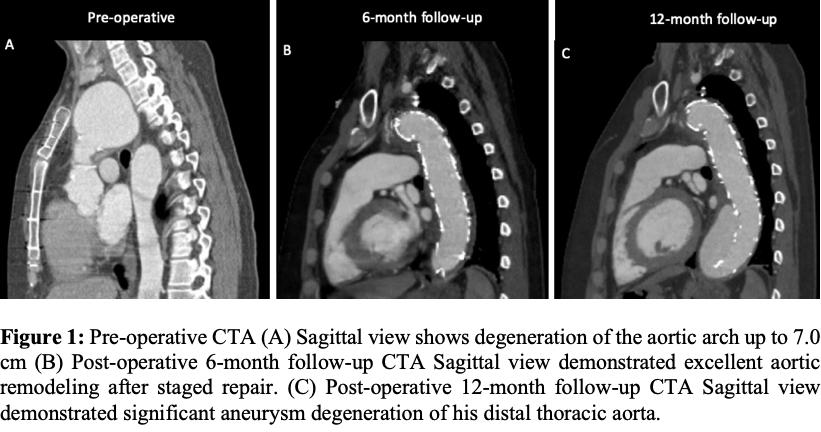
Plan: A left carotid-subclavian artery transposition was performed using felt wrapping due to extremely friable tissue. Two days later he underwent a Zone 2 aortic arch replacement and frozen elephant trunk with a Thoraflex graft® via redo-sternotomy, right axillary artery cannulation and percutaneous left common femoral artery access. Anastomoses were reinforced with felt given the quality of the tissue. After a prolonged hospitalization including a spontaneous retroperitoneal hematoma he was discharged home. Three months later, he underwent an uncomplicated TEVAR to the level of the celiac artery via unilateral percutaneous access. The patient was discharged on post-operative day two. Follow-up was documented at 1 month, 6 months, and 12 months. At 6-month follow-up, his CTA demonstrated complete sac regression of his arch aneurysm, however by 12-month follow-up he had new severe degeneration of his distal thoracic aorta. (Fig 1). Therefore, the patient is in planned for an open TAAA repair to complete a total aortic replacement.
Discussion: This is the first reported case of a patient with confirmed genetic mutation for both LDS and vEDS. Despite historic fear for the risk of operating on patients with these conditions, this case demonstrates that a multidisciplinary approach can be performed safely and that percutaneous access can be accomplished without access site complications. Close follow-up is critical given the risk for further aneurysmal degeneration.