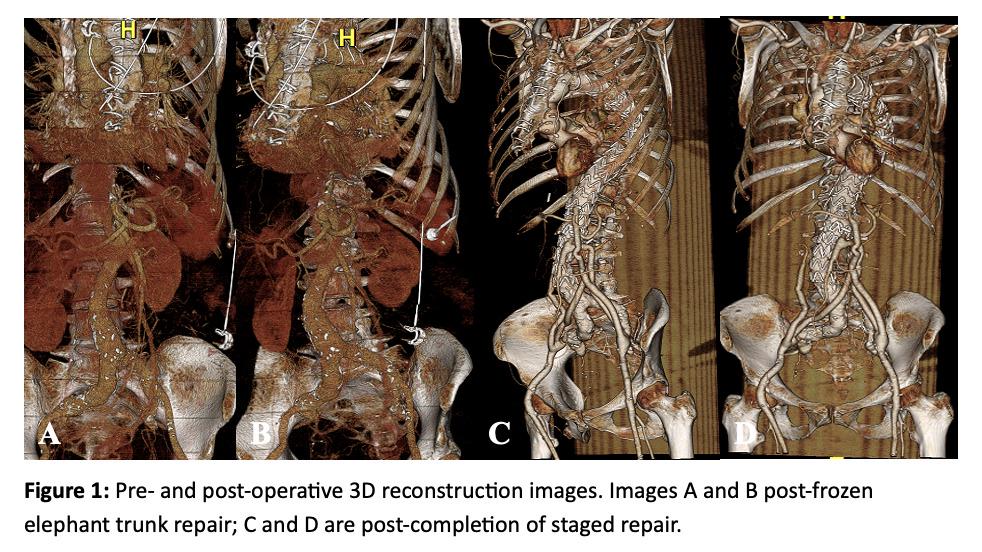
DEMOGRAPHICS: A 69-year-old female with COPD, hypertension, and a Type A dissection repaired 1 year ago elsewhere with a short ascending aortic graft, presented with an 8.5 cm Type II TAA with chronic dissection. HISTORY: Repair of TAAs after Type A or B dissections poses significant risks of spinal cord, mesenteric, and renal ischemia. Although staged proximal to distal repair of the aorta necessitates several procedures, this approach may reduce end-organ ischemia and its sequalae, specifically paralysis. On presentation, due to the size of her aneurysm, this patient developed pulmonary compression requiring intubation. PLAN: To urgently repair her TAA with dissection, she first underwent placement of a 30 x 34 x 150mm Thoraflex® elephant trunk, with a plan to sequentially replace the remaining diseased aorta. Postoperatively, she developed a symptomatic strangulated femoral hernia requiring surgical treatment, delaying the next planned stage by one month. After CTA imaging (Fig 1A-B), we found her unsuitable for fenestrated repair due to her small overall size, and small visceral/renal arteries (4mm). We repaired her TAA through an abdominal incision with four-vessel debranching using two bifurcated grafts: (i) 14x7mm right external iliac to bilateral renal arteries, and (ii) 14x7mm left external iliac to SMA and celiac Dacron graft. Two days later, her final endovascular stage was completed using a free flow Valiant graft to bridge the Thoraflex to the abdominal aorta, with an adjunct spinal cord drain. The patient was extubated intraoperatively after each procedure and had no complications. She is now approximately 3.5 years post-op and doing very well (Fig 1C-D). DISCUSSION: We report using a frozen elephant trunk, then a staged hybrid 4-vessel debranching followed by an endovascular stent graft in a patient with a large TAA post-Type A dissection repair elsewhere. Hybrid visceral-renal debranching techniques coupled with endovascular repair are a viable alternative when fenestrated technology is not suitable. By staging complete aortic replacement, the risks of spinal cord ischemia, mesenteric, and renal ischemia can be ameliorated. This case reinforces the viability of a multi-stage hybrid endovascular repair for TAAs as a safe and promising choice for treating chronic post-dissection aneurysms.