DEMOGRAPHICS:24-year-old caucasian female with history of asthma,ADHD,and depression presented with diagnosis of recent iliocaval thrombosis in setting of infra-renal inferior vena cava(IVC) agenesis. HISTORY:
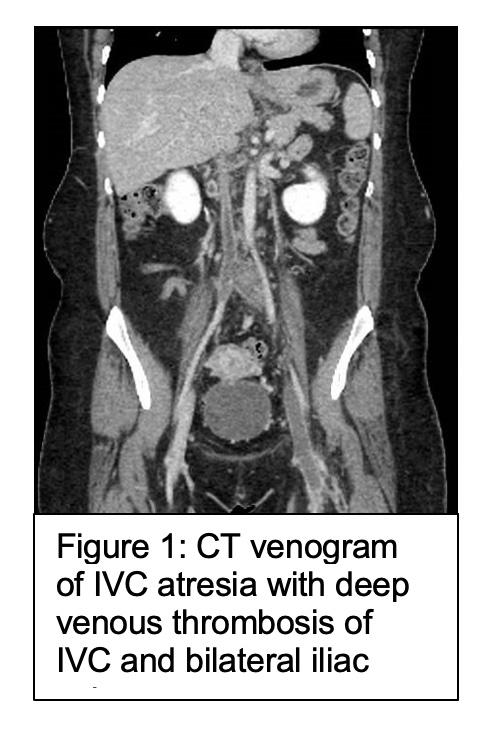
Patient in usual good state of health until one-month prior her left lower-extremity acutely became purple/swollen for 5 minutes with associated antecedent back pain.No prior history of leg swelling,DVT,or other chronic vascular conditions.CT/contrast venography at outside-hospital revealed IVC-agenesis based on venogram finding of collateralization around mid-IVC (Figure 1). Patient discharged on Eliquis and presented to our clinic due to continued severe limitations in mobility from left leg swelling/discomfort necessitating use of walker.
PLAN: Plan was to proceed with thrombolytic therapy for iliocaval thrombotic occlusion through a step-wise approach.
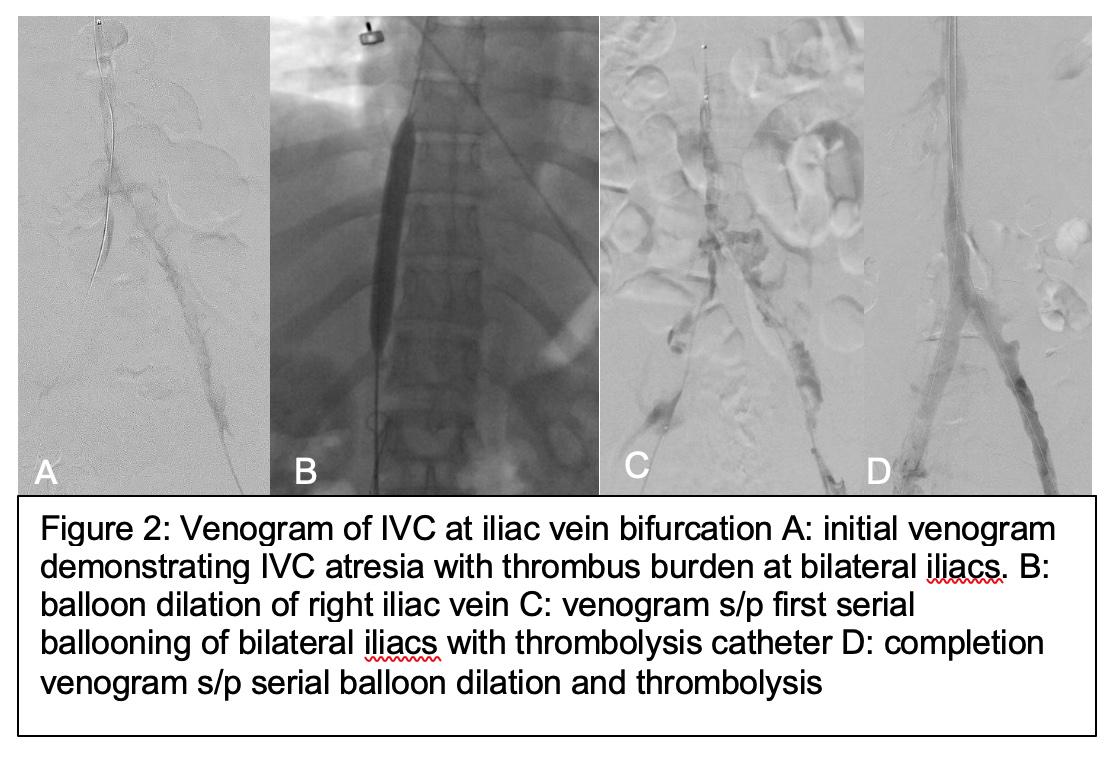
DISCUSSION: Initial venogram revealed thrombosis of left femoral vein, bilateral common iliacs(CIV),and infrarenal IVC with placement of lysis-catheters in bilateral iliacs(heparin 250units/hr and tPA 0.5mg/hr).Lytic therapy limited by drop in fibrinogen levels for which thrombolytic therapy was stopped and saline was infused with continued systemic anticoagulation.Following day, selective angiogram revealed significant clearance of thrombus within main central channel of iliac veins/IVC,but absent antegrade in-line flow through iliocaval system.Aspiration mechanical thrombectomy was performed of IVC, bilateral CIV/EIV using Penumbra CAT12 Lightning device.Balloon angioplasty then performed on IVC with sequential dilation to 14mm using Armada-balloons and repeat placement of lysis-catheter in bilateral CIV/IVC(20cm-McNamara on right, 30cm-McNamara on left using high-volume heparin 100cc/hr due to recent fibrinogen-drop).On third-consecutive operating day,lysis-catheters removed with bilateral CIV/IVC angioplasty and improved venous flow. Patient discharged next-day on Eliquis.Patient did well post-operatively with resolve of symptoms and ambulating independently.One-month later,patient re-assessed for residual stenosis with repeat venography demonstrating widely patent IVC/bilateral iliacs with residual retrohepatic-cava stenosis treated with balloon angioplasty to 14mm (Figure 2). At 3-month follow-up, patient continues to be asymptomatic and have patent flow on CT venogram/duplex imaging while on Eliquis.Plan for repeat venography in 1-year and consider anticoagulation cessation, if appropriate.