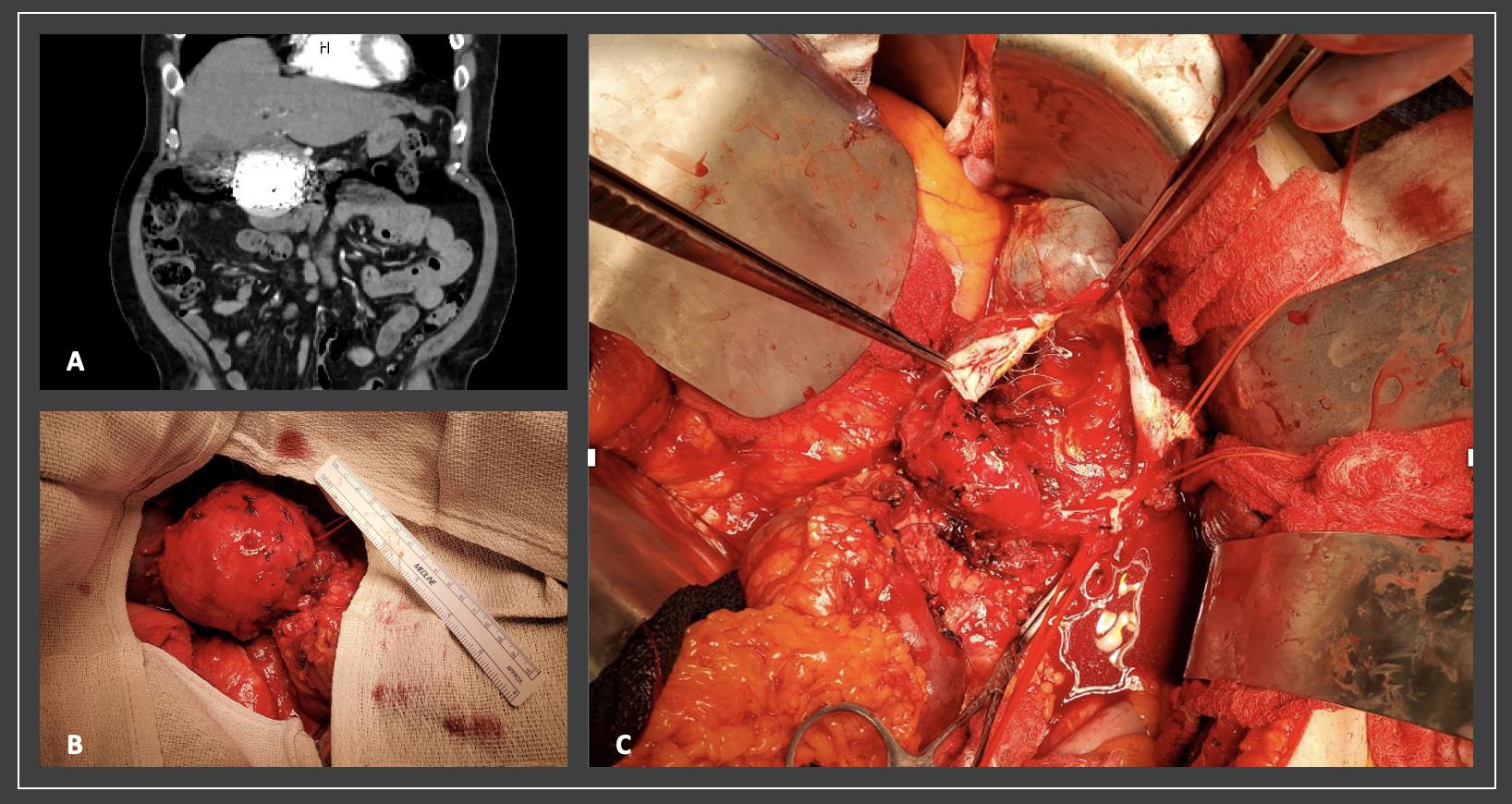
DEMOGRAPHICS: 77-year-old Caucasian male. HISTORY: A 77-year-old male referred to us after an incidentally found 3.7 cm gastroduodenal artery aneurysm (GDAA). He consented to endovascular management of his GDAA that had grown to 5 cm. Despite radiographic success at coil embolization and a year of stabilization in size, surveillance imaging revealed continued growth to 8 cm with involvement of the hepatic confluence due to degeneration of the GDAA neck. (Figure 1A) PLAN: Operative intervention was pursued. After gaining access to the lesser sac, the celiac axis was identified and controlled at its origin. Due to the significant size of the aneurysm, there was significant involvement of the duodenum and pancreas. The aneurysm was noted to extend up to its takeoff from the hepatic artery. The hepatic bifurcation was identified and controlled. Kocherization allowed for full circumferential exposure of the GDAA. (Figure 1B) The SMA was identified inferior to the pancreas. Great saphenous vein was harvested as the GDAA neck had notable degeneration at its origin.Once heparinized, the left and right hepatic artery branches and origin were occluded with noticeable lack of pulsatility within the GDAA. The aneurysm sac was opened and debulked. (Figure 1C) Bile was noted while taking down the wall as the aneurysm had incorporated the common bile duct (CBD). We elected to perform a primary end-to-end anastomosis of a redundant hepatic artery with appropriate flushing prior to repair of a lateral defect of the CBD over a 7 Fr biliary drain. Flow was reestablished and confirmed with doppler prior to closure. Postoperatively, the patient developed a type B pancreatic fistula managed conservatively prior to eventual progression of diet and discharge. DISCUSSION: Endovascular intervention has evolved into the gold standard for accurately diagnosing and therapeutically addressing GDAAs. This patientís GDAA exhibited continued growth despite a perceived successful coil embolization and one year of size stabilization. This case demonstrates the importance of long-term surveillance in addition to a viable strategy during his open intervention sparing the patient from a potentially fatal rupture.