DEMOGRAPHICS: We present a Caucasian 71 year old man with history of right transradial carotid stent placed at the time of his coronary artery bypass graft 17 years prior to presentation.
HISTORY: Patient presented to our hospital with left upper and lower extremity weakness and numbness, and hypertensive urgency. Patient reported a multiple month history of recurrent, transient left sided weakness and aphasia that was increasing in frequency. CTA Neck Revealed a high-grade in-stent restenosis of his carotid stent, and the distal aspect of the stent extended to the C2 vertebrae.
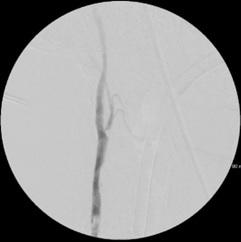
PLAN: We performed a Right Transcarotid Arterial Revascularization. A completion angiogram of the neck revealed a subtle filling defect associated with the tip of the flow reversal device. We assessed the flow reversal, which was now sluggish. Through a separate incision, we obtained vascular control of the distal common carotid and performed an embolectomy of the common carotid artery. We were able to re-establish flow reversal. Completion neck and cerebral angiogram showed no filling defect. Patient had no post-operative neurologic deficit and cessation of his transient ischemic attacks. DISCUSSION: Transcarotid Arterial Revascularization is a viable treatment option for symptomatic carotid in-stent restenosis. We identified his common carotid embolus due to a subtle filling defect associated with our flow reversal catheter and poor flow reversal after stent placement. If we had not appreciated these findings, he would have likely suffered a devastating stroke. We hope to highlight a rare complication of an evolving surgical technique, and how to identify this complication when it occurs.