DEMOGRAPHICS: A 73-year-old female former smoker with hypertension, peripheral artery disease, and hyperlipidemia, presented with an inferior pancreaticoduodenal artery aneurysm (IPDAA).
HISTORY: The patient presented to the vascular clinic after a computed tomography (CT) scan for workup of microhematuria showed a 2.3 x 2.2 cm mass anterior to the aorta above the level of the left renal vein concerning for an IPDAA (Figure 1A). She had palpable distal pulses and no abdominal tenderness.
PLAN: She underwent mesenteric angiography which revealed an occluded celiac artery and a 2.5 cm aneurysm arising from the IPDA at its origin from the superior mesenteric artery (SMA). The aneurysm outflow had a large collateral supplying the liver, spleen, and stomach (Figure 1B). Embolization was deferred given the risk of hepatic ischemia. She underwent a supraceliac aorto-hepatic bypass with an 8-mm Rifampin-soaked Dacron graft. Dissection of the aneurysm sac was not possible given its location posterior to the pancreas. After bypass completion, she was taken directly for angiography and aneurysm embolization using interlocking coils. Completion angiography showed no aneurysm filling (Figure 1C). On postoperative day (POD) 2, her hemoglobin dropped from 12 to 6 with associated hypotension. CT angiography showed a patent bypass graft and contrast within the residual aneurysm. Repeat angiography showed ongoing perfusion of the aneurysm. Five additional interlocking coils were deployed within the aneurysm. An 8 x 2.5 cm Viabahn stent was placed in the SMA. Completion angiography showed no additional perfusion to the aneurysm. Distal SMA branches were widely patent. The remainder of her hospitalization was unremarkable. She was discharged on POD 4 on Plavix for 6 months and aspirin 81mg long-term. At follow-up, she was recovering expectantly. 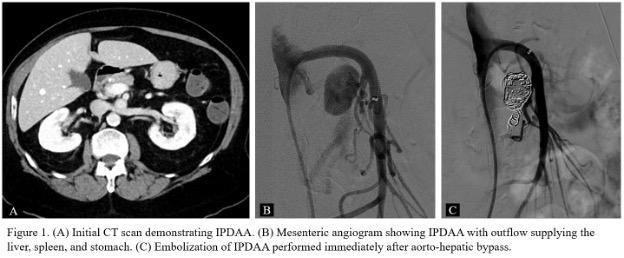
DISCUSSION: PDAAs represent approximately 2% of all visceral artery aneurysms with a risk of rupture up to 50%. IPDAAs in association with celiac artery disease are a known entity. Endovascular repair is preferred as it is less invasive and less morbid. When surgical repair is performed, the aneurysm itself is usually repaired or excised. This case is unique given the patientís anatomy and hepatic blood flow, which required a combined endovascular and surgical approach.