|
Back to Annual Symposium Program
Combined use of an endovascular stent graft and ultrasound-guided thrombin injection in the management of an iatrogenic subclavian pseudoaneurysm and arteriovenous fistula
Daniel E. Ramirez, MD, W C. Sternbergh, III, MD, Taylor Smith, MD, Hernan A. Bazan, MD.
Ochsner Medical Center, New Orleans, LA, USA.
Objectives:Vascular injury during central venous access is a rare but serious complication. Multiple reports have highlighted the use of stent grafts in the management of arterial trauma; more complex central vessel injury may require a multi-modality treatment strategy, particularly the use of ultrasound-guided thrombin injection. We report the minimally-invasive management of a patient who had recently undergone an orthotopic liver transplant presenting with a pulsatile neck mass after central venous catheter placement who sustained 1) a pseudoaneurysm of the right subclavian artery just distal to the origin of the right vertebral artery and 2) an arteriovenous fistula between the right subclavian artery and the brachiocephalic vein.
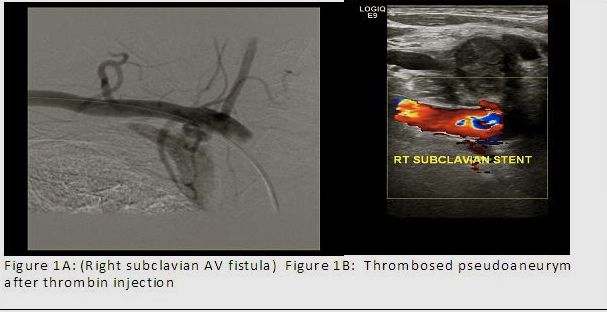
Methods: Selective right sublclavian angiography demonstrated a pseudoaneurysm arising from the proximal right subclavian artery just distal to the takeoff of the right vertebral. On delayed imaging, an arteriovenous fistula to the right brachiocephalic vein was noted (Fig. 1A). The right vertebral artery was selected with a 0.014 inch wire to help with vessel orientation and have a platform to stent as a ‘bail-out’ should the vertebral artery be inadvertently covered. Next, a 10 mm x 38 mm balloon-expandable stent graft was placed in the right subclavian artery just distal to the origin of the right vertebral artery. Post-stent deployment with a 12 mm semi-compliant balloon ceased the flow into the arteriovenous fistula. Filling of the right subclavian artery pseudoaneurysm continued, despite reversal of anticoagulation. Surveillance ultrasound within a week post-procedure, demonstrated flow into the pseudoaneurysm. Emanating a proximal endoleak near the origin of the right vertebral artery. The pseudoaneurysm had grown in size (> 0.5 cm) in a week since the stent graft was deployed. Thrombin (300 u) was then injected into the aneurysm sac under ultrasound-guidance.
Results: Complete and immediate thrombosis was noted after thrombin injection and this thrombosis has persisted on 6-month follow-up; patient has been asymptomatic from the AVF and thrombosed pseudoaneurysm.
Conclusions: Despite precise covered stent graft placement in the management of arch vessel injury, endoleaks may occur with persistent flow. Salvage ultrasound-guided percutaneous thrombin injection may be invaluable in select patients. 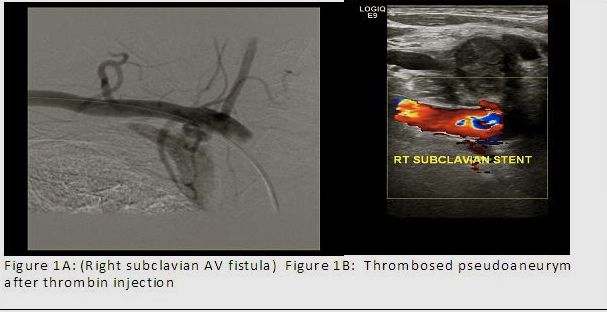
Back to Annual Symposium Program

|