|
Back to Annual Symposium Program
Hybrid approach to bleeding aorto-enteric fistula in patients not amenable to traditional open repair using the renal artery as a conduit.
Guillermo A. Escobar, MD, Jonathan L. Eliason, MD, Justin B. Hurie, MD.
University of Michigan, Ann Arbor, MI, USA.
Objectives:
Survival from bleeding abdominal aorto-duodenal fistula is time-dependent and current management mandates open repair of the aorta and the intestinal defect. Surgery may be contraindicated, or too high risk in some patients due to comorbidities or complex abdomens. Endovascular repair of the aorta requires large diameter access to the aorta which also may not be available.
Methods:
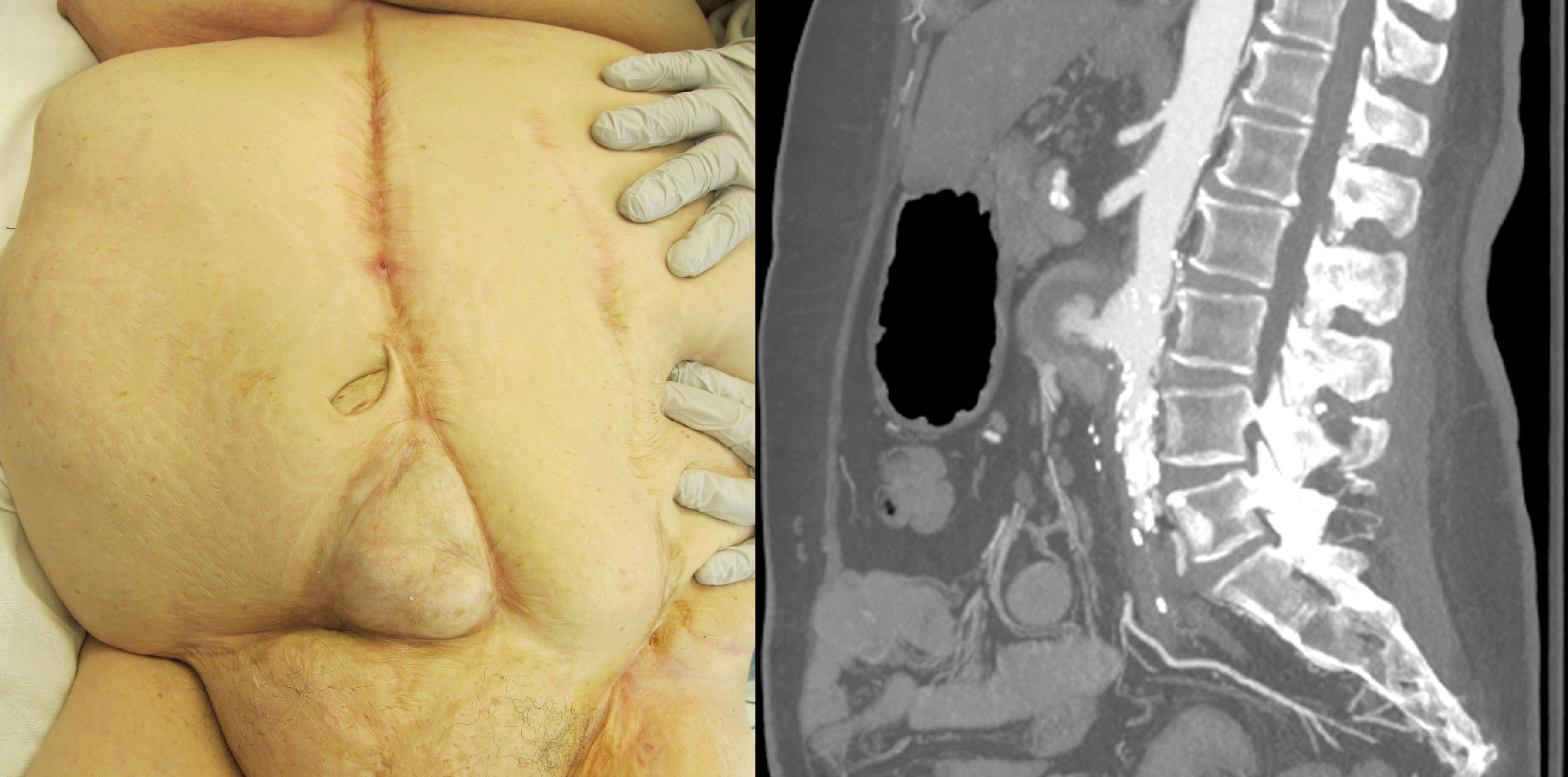
A 66 year old female with sudden-onset hematemesis, hematochezia and fainting was diagnosed with hemorrhagic shock from an aorto-enteric fistula. On arrival to our center she was found to have a surgical history notable for several unknown transabdominal vascular procedures, multiple transabominal hernia repairs and bowel resections culminating in a skin graft over bowel. She had dense, bilateral groin scars that were partially healed. CTA revealed a large, pseudoaneurysm from the infrarenal aorta extravasating into the duodenum. The 14mm aorta terminated directly into the right internal iliac artery. She had occluded left common iliac, left internal iliac (IIA), bilateral external iliac and common femoral arteries. She reconstituted her profundas via collaterals. Her left renal artery was only patent at the origin, and the kidney was atrophic. Her creatinine was 1.4mg/dL.
Via a retroperitoneal approach, supraceliac control was obtained. The left renal artery was amputated and a 8mm Dacron conduit was anastomosed and externalized. The angiogram was impaired due to the use of a mobile C-arm, her lateral position and obese habitus, so a catheter was placed in the right renal artery to mark the proximal limit of deployment. A 16mm x 8.5cm AneuRx graft limb was soaked with Rifampin, deployed and successfully sealed the large pseudoaneurysm.
Results:
While duodenoscopy at one month identified residual graft (from a presumed aortic patch angioplasty) in the duodenum, the patient was discharged home with suppressive antibiotics on a regular diet without SIRS or bleeding for 3 months so far.
Conclusions:
Endovascular exclusion of bleeding aorto-enteric fistula by any means may be lifesaving. The second stage repair of the enteric defect may thus be delayed to allow for patient stabilization and optimization, or just obviated in patients whose comorbidities make open repair unreasonable. 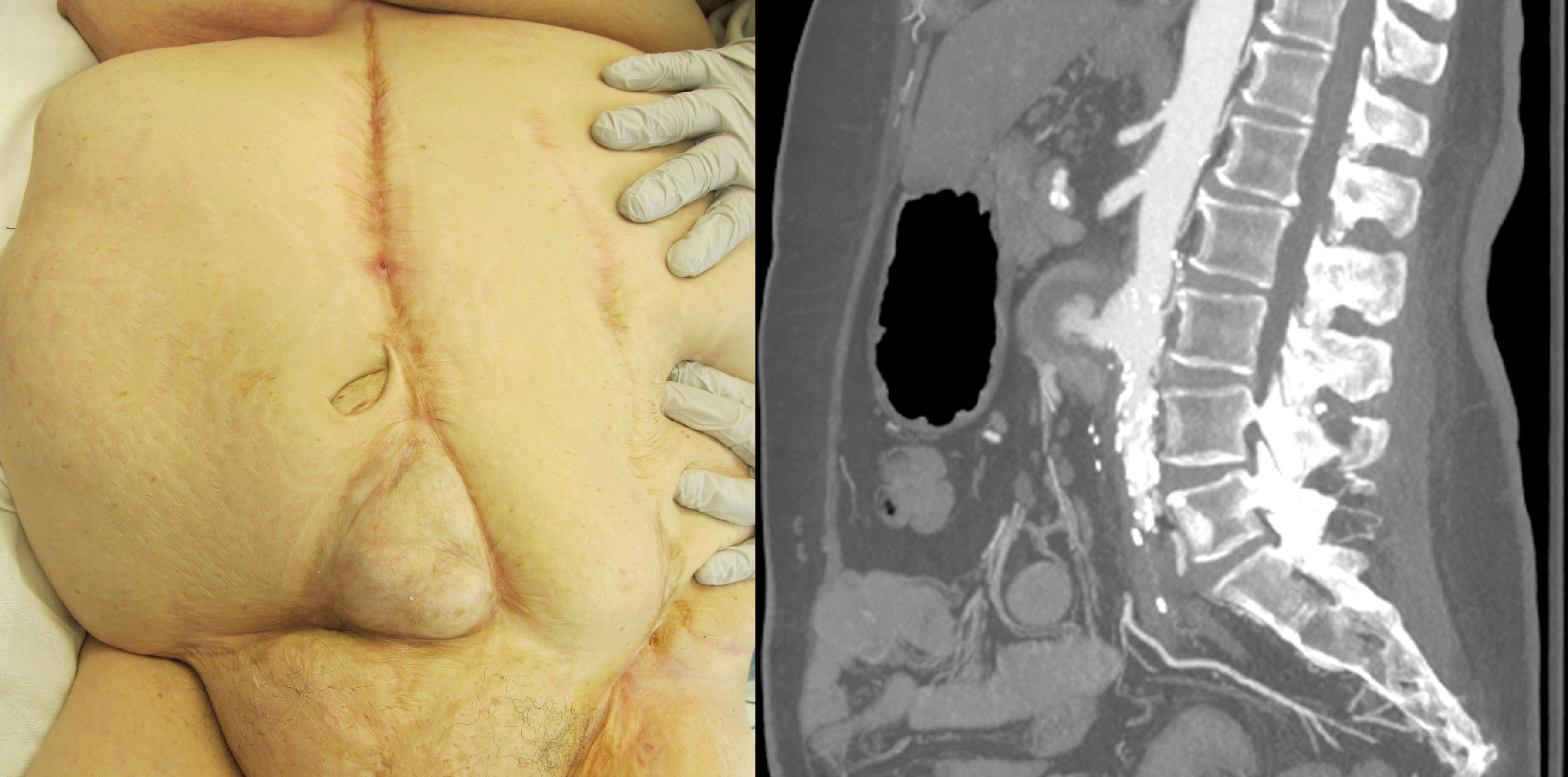
Back to Annual Symposium Program

|