|
|
 |
Back to Annual Symposium Program
Isolated Iliac Artery Aneurysms: Management and Outcomes in the Endovascular Era
Rodney P. Bensley, MD, Rob Hurks, MD, Ruby C. Lo, MD, Frank Pomposelli, MD, Allen Hamdan, MD, Mark Wyers, MD, Elliot Chaikof, MD, Marc Schermerhorn, MD.
BIDMC, Boston, MA, USA.
Objectives:
Isolated iliac artery aneurysms (IAA) are uncommon. Treatment is undertaken to prevent rupture and its’ high accompanying mortality rate. We sought to examine the management and outcomes of isolated IAA since the introduction of endovascular repair.
Methods:
We identified all patients undergoing open surgical repair or endovascular repair of isolated IAA in the Nationwide Inpatient Sample from 1988-2009. A primary diagnosis of an IAA was required. We excluded patients with diagnoses of aortic aneurysms as well as those undergoing aortic aneurysm and/or aortic dissection repair. We examined trends in management during this period and compared in-hospital deaths and postoperative complications between open and endovascular repairs for the years 2000 to 2009.
Results:
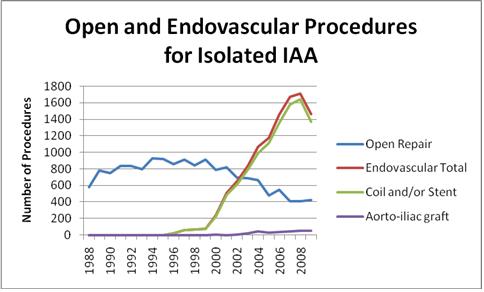
We identified 15,851 open surgical repairs and 10,978 endovascular repairs. Endovascular repairs increased steadily and surpassed open repair in 2003. The majority of endovascular repairs were coil embolization and/or peripheral stent placement with the remaining cases consisting of aortoiliac stent grafts with and without coil embolization and/or an additional peripheral stent (Figure 1). Patients undergoing endovascular repair were older (72.2 vs. 69.2 years, <0.001) with more coronary artery disease (41.7% vs. 32.3%, <0.001), prior myocardial infarctions (12.5% vs.10.0%, <0.02), and chronic renal failure (7.3% vs. 4.0%, <0.001). Patients undergoing open repair had significantly higher in-hospital mortality (7.1% vs. 1.0%, <0.001) and postoperative complications: cardiac complications (5.6% vs. 1.7%, <0.001), respiratory complications (16.0% vs. 2.3%, <0.001), renal failure (10.8% vs. 3.4%, <0.001), hemorrhage (6.4% vs. 4.0%, <0.01), wound dehiscence (1.0% vs. 0.2%, <0.01), and wound infections (1.6% vs. 0.3%, <0.001). Patients undergoing open repair were less likely to be discharged home (77.0% vs. 92.7%, <0.001) and had a longer median length of stay (6.0 vs. 2.0 days, <0.001).
Conclusions:
Isolated IAA are uncommon. Treatment has shifted away from open surgical repair towards less invasive endovascular techniques and their lower morbidity and mortality. This is similar to the trend seen with abdominal aortic aneurysm (AAA) repair. However, mortality with open repair of isolated IAA remains higher than that with open repair of infrarenal AAA. 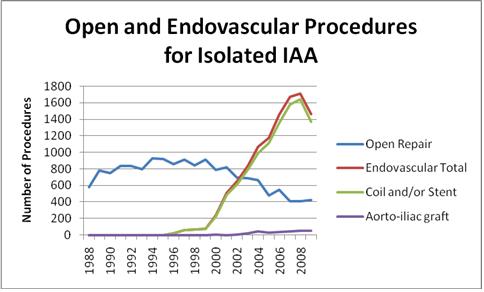
Back to Annual Symposium Program

|