|
Back to Annual Symposium Program
High Intraoperative Transfusion Volumes are Independently Associated with a Higher 30-day Mortality in Stanford Type-A Aortic Dissection Patients
Wadi Gomero-Cure, M.D., John J. Ricotta, M.D., Sean O'Donnell, M.D., Fred Beavers, M.D., Paul Corso, M.D., Robert Lowery.
Washington Hospital Center / Georgetown Univ Hospital, Washington, DC, USA.
Objectives: Crystalloid, blood, and plasma-rich transfusion products are known to independently impact mortality, surgical outcomes, organ failure, acute lung injury, and nosocomial infection rates in various surgical and non-surgical populations. Conservative transfusion practices have recently shown benefit in the critically-ill and trauma populations. Little is known about the impact current transfusion practices have on outcomes of Stanford Type-A aortic dissection patients. Our aim is to identify if crystalloid, blood, plasma-rich products, or the summation of all products transfused during the operative intervention impacts 30 day mortality in this type-A dissection patients.
Methods: 152 Stanford Type-A aortic dissection patients treated over a 4 year period at a single institution were retrospectively analyzed using prospectively collected data. Blood, plasma-rich product, and crystalloid volumes transfused by anesthesiology and/or perfusionists during the operative intervention were obtained from a database collected by research associates. Univariate and multivariate logistic regression was used to examine the odds ratio of 30-day mortality for patients receiving various volumes of products to compare potential risk factors. T test,Wilcoxon rank sum test, and chi-square test were used to compare the differences between groups. General linear model was used to assess the association of length of ICU stay with volume of blood transfused. All p values were two-side, and <0.05 was considered statistically significant.
Results: High crystalloid, blood, and plasma-rich intraoperative transfusion volumes are each an independent risk factor for 30 day mortality. Overall high transfusion volume over 7 Liters (adding crystalloid, blood, plams-rich products) is an independent risk factor for 30 day mortality.
Conclusions: High intraoperative transfusion volumes are associated with worst overall 30-day mortality after adjusting for age and gender in surgically treated Type-A aortic dissection patients. Clinicians who care for these patients should bear these risks in mind when considering resuscitation and judicious transfusion practices should be encouraged. Further research on the mechanisms by which transfusion components promote these effects are required to ultimately improve surgical outcomes. 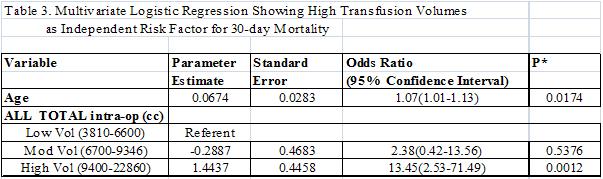
Back to Annual Symposium Program

|

