Back to ePosters
Functional Status of Elderly Adults before and after Abdominal Aortic Aneurysm Repair
Todd R. Vogel, MD, MPH, Gregory F. Petroski, PhD, Robin L. Kruse, PhD.
University of Missouri Hospital & Clinics, Columbia, MO, USA.
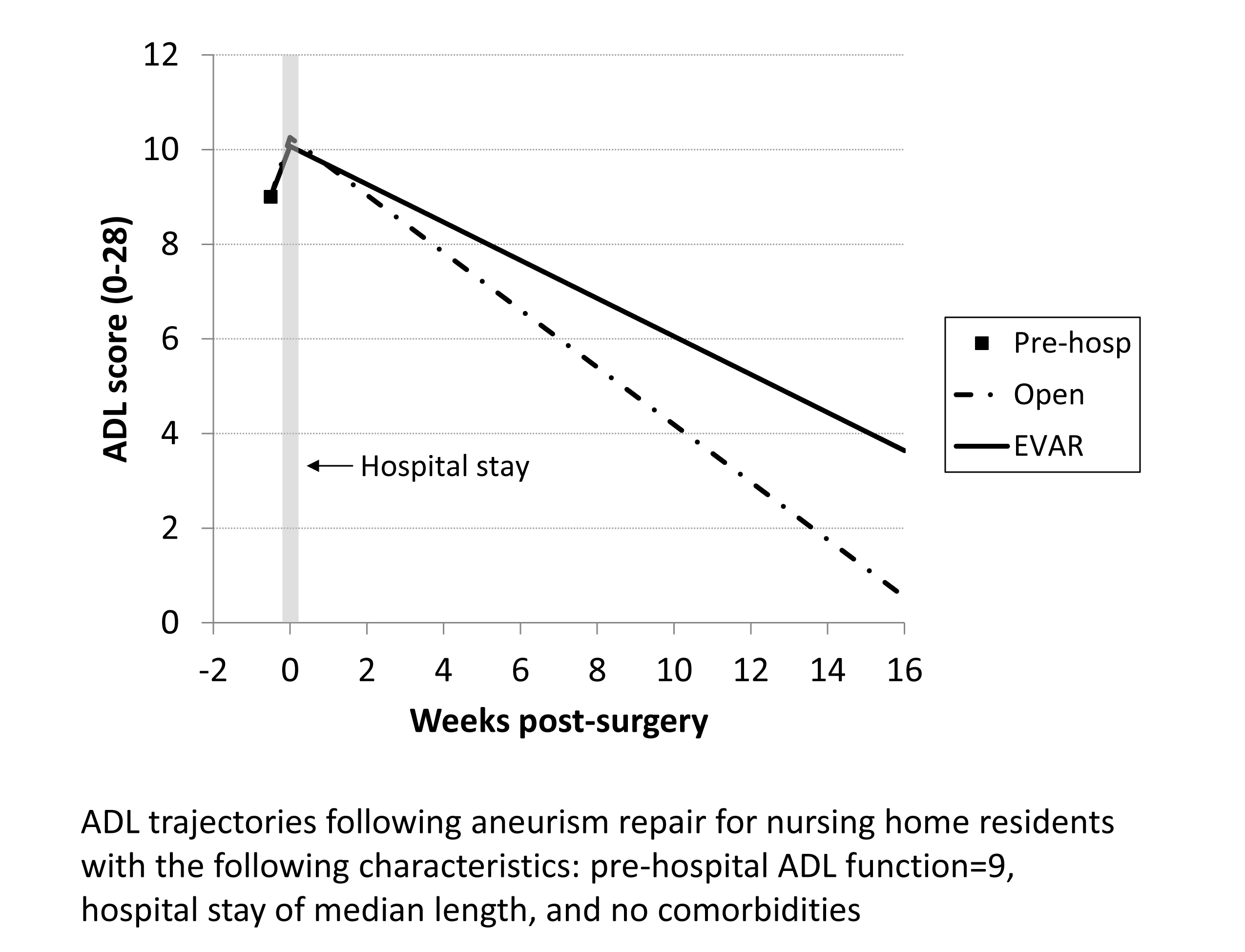
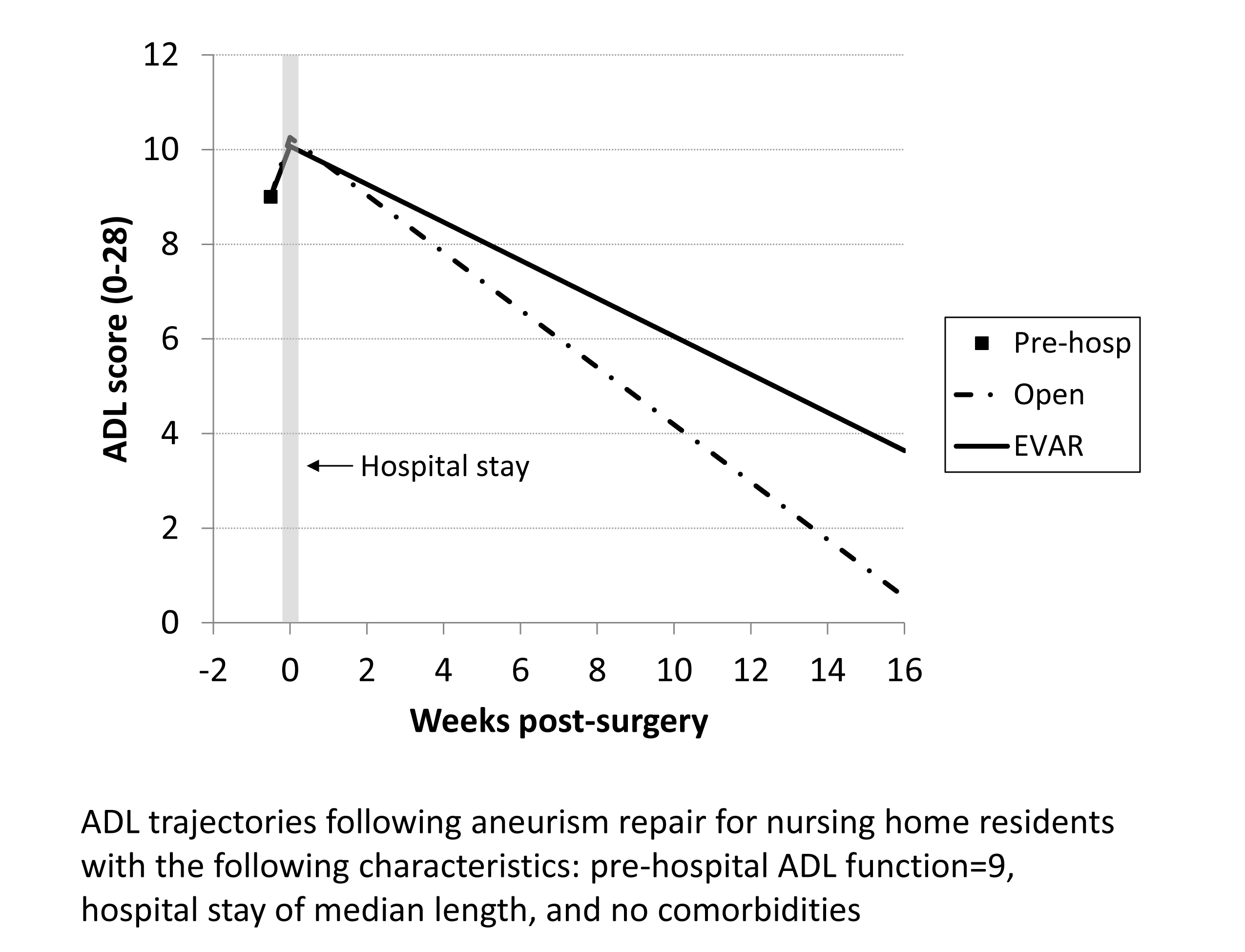
Objectives: Although many trials have evaluated Abdominal Aortic Aneurysm (AAA) repair, the impact of these procedures on the functional status in the frail elderly is not well described. The effects of elective open AAA repair (OAR) or endovascular AAA repair (EVAR) and comorbidities were evaluated for their impact on functional trajectories after discharge.
Methods: Medicare inpatient claims were linked with nursing home (NH) assessment data to identify elective admissions for EVAR and OAR. A functional score (0-28; higher indicating greater impairment) based on activities of daily living (ADL) was calculated before and after interventions. A logistic regression was used to develop a propensity score for receiving EVAR as residents were not randomized. Hierarchical linear modeling determined the effect of surgery on residents’ function, controlling for pre-hospital function, hospital length of stay (LOS), stroke, and the propensity score.
Results: 161 residents underwent EVAR and 52 residents underwent OAR. 65.3% were men and 62.0% were from 76 to 85 years old. Mean LOS was 8.3 days for OAR and 5.1 days for EVAR. Prior to hospitalization, 47.4% of residents had good function (ADL score 0-10), and 48.4% were moderately impaired (ADL score 11-20). Compared to pre-hospital function, disability was greater following hospital discharge and subsequently improved. Higher baseline ADL score, increased LOS, and stroke were associated with worse trajectories. Procedure type was not significantly related to post-surgery impairment scores or the subsequent rate of improvement. By 120 days following hospital discharge, 6 residents had died, 65 were readmitted to the hospital, 56 remained in the NH, 79 were discharged to home or assisted living, and 7 lacked follow-up data.
Conclusions: OAR and EVAR were associated with similar initial declines and comparable post operative trajectories suggesting that less invasive EVAR was not associated with improved functional preservation compared to OAR. LOS was found to be higher than expected in the frail elderly after EVAR; longer stays were associated with poorer functional trajectories. Higher baseline ADL scores were significantly associated with inferior functional status after both procedures. Evaluation of preoperative function may assist physicians in predicting patient-centered outcomes in this high risk population.
Back to ePosters

|