Heel Wounds Predict Poor Outcomes After Infrapopliteal Revascularization
Abhisekh Mohapatra, MD, Jon C. Henry, MD, Efthymios D. Avgerinos, MD, Rabih A. Chaer, MD, Steven A. Leers, MD, Aureline Boitet, MD, Michael J. Singh, MD, Eric S. Hager, MD.
University of Pittsburgh Medical Center, Pittsburgh, PA, USA.
Objective: Ischemic heel ulcerations are generally thought to carry a poor prognosis. We hypothesized that patients undergoing infrapopliteal revascularization for heel wounds, either bypass or endovascular intervention, would have lower wound healing rates and amputation-free survival than patients with forefoot wounds.
Methods: Retrospective chart review was performed of patients who presented between 2006 and 2013 to our institution with ischemic foot wounds and infrapopliteal arterial disease and underwent either pedal bypass or endovascular tibial artery intervention. Data was collected on patient demographics, comorbidities, wound characteristics, procedural details, and postoperative outcomes, then analyzed by initial wound classification. The primary outcome was major amputation or death.
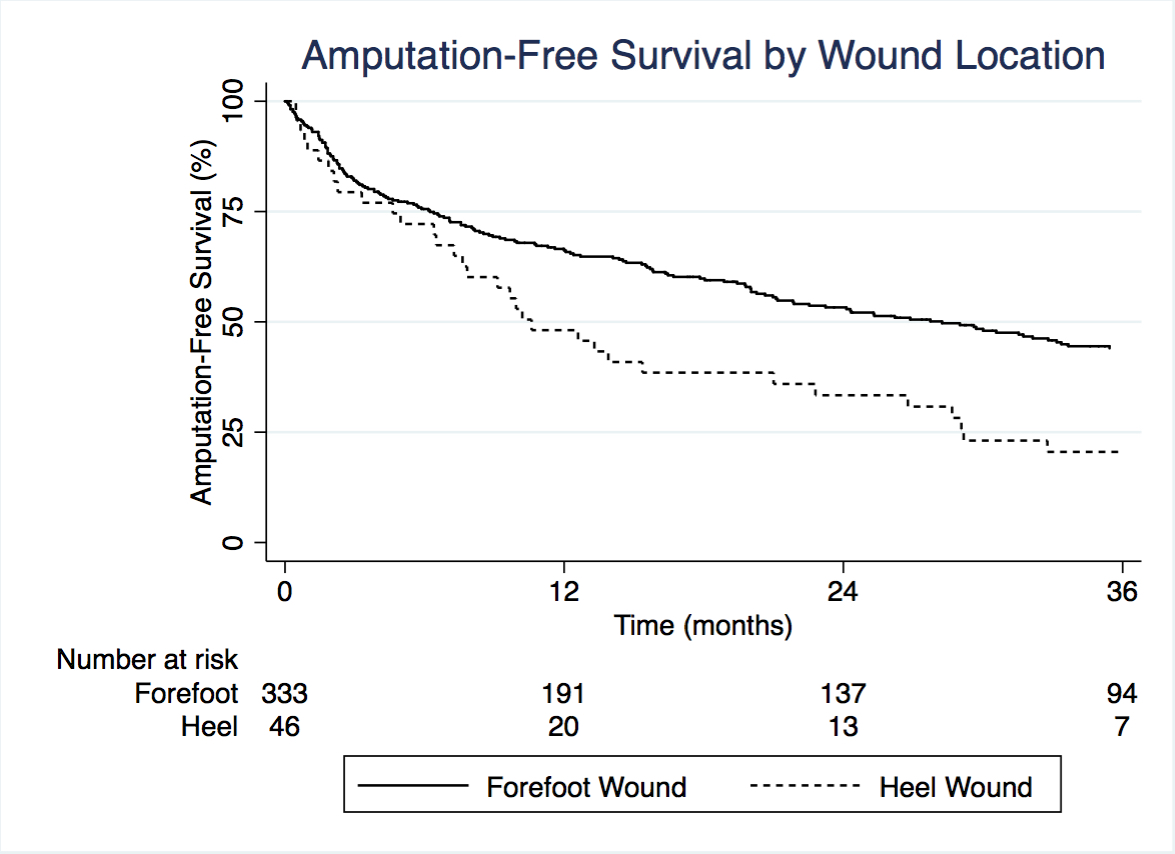
Results: 398 limbs underwent treatment for foot wounds; accurate wound data was available in 380 cases. There were 101 bypasses and 279 endovascular interventions, with mean follow-up 24.6 and 19.9 months, respectively (P = .02). Heel wounds comprised 12.1% of the total with the remainder being forefoot wounds; there was no difference in treatment modality by wound type (P = .94). Of 46 heel wounds, 5 (10.9%) had clinical or radiographic evidence of calcaneal osteomyelitis. Patients with heel wounds were more likely to have diabetes mellitus (P = .03) and renal insufficiency (P = .004). 36.9% of wounds healed within one year, with no difference by wound location (P = .30). Endovascular treatment was associated with improved healing of forefoot wounds (P = .02) but not heel wounds (P = .14). Major amputation rate at one year was 17.8%, with no difference by wound location (P = .81) or treatment type (P = .33). Three-year major amputation-free survival was 43.8% with a forefoot wound and 20.8% with a heel wound (P = .03). In a multivariate analysis, heel wounds and endovascular intervention were both predictors of major amputation or death; however, there was significant interaction such that bypass improved outcomes in patients with forefoot wounds (HR 1.97, P < .001) but not those with heel wounds (HR 0.79, P = .53).
Conclusions: Patients presenting with heel ulceration who undergo infrapopliteal revascularization are prone to lower amputation-free survival, despite equivalent wound healing and regardless of treatment modality.
Back to 2017 Program




