Pre-operative Risk Factors Predict Increased Risk for Stroke after Carotid Endarterectomy
Anam Pal, MBBS1, Saqib Zia, MBBS1, Kuldeep Singh, MD1, Jonathan S. Deitch, MD1, Eitezaz Mahmood, BA2, Maria Sfakianos, MD3, Jonathan Schor, MD1.
1Staten Island University Hospital, Staten Island, NY, USA, 2Feinberg School of Medicine, Northwestern University, Chicago, IL, USA, 3North Shore University Hospital, Manhasset, NY, USA.
Introduction: Stroke after Carotid Endarterectomy (CEA) is a devastating event. There is a need for predictive models to identify patients at high risk for stroke. We sought to use a large multi-institutional database in order to examine preoperative risk factors for developing stroke after CEA.
Methods: The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) carotid endarterectomy targeted files were queried from 2011-2014. The primary outcome was 30-day stroke. A multiple logistic regression was used, controlling for demographic factors, preoperative comorbidities and clinical characteristics. The model was then tested to estimate the receiver operating curves (ROC) and goodness of fit.
Results: A total of 13,846 patients were included in our analysis. 289 (2.09%) of these patients had a stroke. The mean age of our sample was 70.5 years. 61% of our patients were male and the most common comorbidities included hypertension requiring medication (84.0%), diabetes (30.0%), dyspnea (13.3%), chronic obstructive pulmonary disease (10.1%), and congestive heart failure (1.3%). Risk-adjusted multiple regression indicated that preoperative stroke/transient ischemic attack (odds ratio [OR] 2.78, p<0.0001), stenosis of contralateral carotid artery >80% (OR 2.20, p<0.0001), transfer status other than from home/nursing home/chronic care/intermediate care, (OR 2.08, p<0.0007), and hypertension requiring medications (OR 1.79, p<0.0041) were statistically significant predictors for stroke. The c-statistic for our model was at 0.72. The Hosmer-Lemenshow goodness-of-fit statistic was 0.99.
Conclusion: We identified preoperative factors that predict stroke after CEA. While hypertension appears to be predictive, other medical co-morbidities are not predictive of stroke after CEA. Symptomatic patients and patients with contralateral disease appear to be at highest risk of stroke after CEA.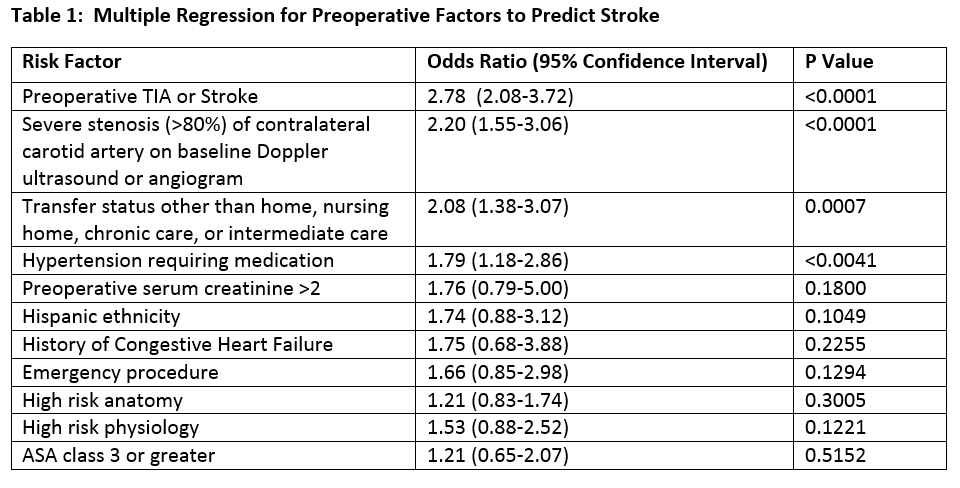
Back to 2017 Karmody Posters




