Preoperative Anemia a Risk Factor for Adverse Outcomes following Infrainguinal Bypass Surgery in Patients with Chronic Limb-threatening Ischemia
Thomas C.F. Bodewes, MD1, Alexander B. Pothof, MD MSc1, Jeremy D. Darling, BA1, Gabrielle N. Yee1, Katie E. Shean, MD1, Sarah E. Deery, MD1, Frans L. Moll, MD PhD2, Marc L. Schermerhorn, MD1.
1Beth Israel Deaconess Medical Center, Boston, MA, USA, 2University Medical Center, Utrecht, Netherlands.
OBJECTIVES: Preoperative anemia in elderly patients undergoing surgery is prevalent and associated with adverse events; however, interactions with other risk factors in patients with chronic limb-threatening ischemia (CLTI) are not well described. The purpose of this study was to assess perioperative outcomes of patients undergoing bypass surgery associated with lower hematocrit (HCT) levels on admission.
METHODS: Patients with CLTI undergoing non-emergent infrainguinal bypass surgery were identified in the Targeted Vascular NSQIP 2011-2014. Thirty-day outcomes were stratified based on preoperative HCT levels, into: severe (HCT ≤29%), moderate (HCT 29.1-34%), or mild anemia (HCT 34.1-39%), and patients were compared to no anemia (HCT >39%). Independent associations between perioperative outcomes and preoperative low hematocrit levels were established using multivariable logistic regression. A sensitivity analysis was performed to assess effect modifications between anemia and perioperative blood transfusions.
RESULTS: We identified 5081 patients undergoing bypass surgery, of which 741 (14.6%) had severe, 1317 (25.9%) moderate, 1516 (29.8%) mild, and 1507 (29.7%) had no anemia. Anemic patients were older, less likely male and white, more often had tissue loss, and a greater burden of comorbidities (e.g. hypertension, diabetes, renal insufficiency). Compared to patients without anemia, those with lower hematocrit levels had an increased risk of mortality (no anemia: 0.7% vs. severe: 3.1%, OR:2.8, 95% CI:[1.3-6.3]; vs. moderate: 3.0%, OR:2.6[1.2-5.5]; Table). Severe anemia also proved to be associated with major amputation (6.9% vs. 3.3%, OR:1.6[1.01-2.6]) compared to no anemia. Lower hematocrit levels on admission were additionally associated with other adverse outcomes, including MACE (severe: OR:1.9[1.1-3.0]; moderate: OR:1.9[1.3-2.9]; mild: OR:1.6[1.1-2.4]) and unplanned return to the operating room (severe: OR:1.6[1.2-2.1]; moderate: OR:1.5[1.2-1.8]; mild: OR:1.3[1.03-1.6]). The increased risk of death associated with preoperative anemia was more pronounced in patients receiving perioperative blood transfusions than those who did not (OR:6.5[2.3-18.7]).
CONCLUSIONS: Mortality in CLTI patients undergoing infrainguinal bypass surgery is inversely associated with hematocrit levels, with the highest mortality rates in the most severe anemic patients. The correlation between major adverse events and anemia was stronger in those patients receiving perioperative blood transfusions. Further research should be directed at defining optimal preoperative management in anemic CLTI patients undergoing surgery. 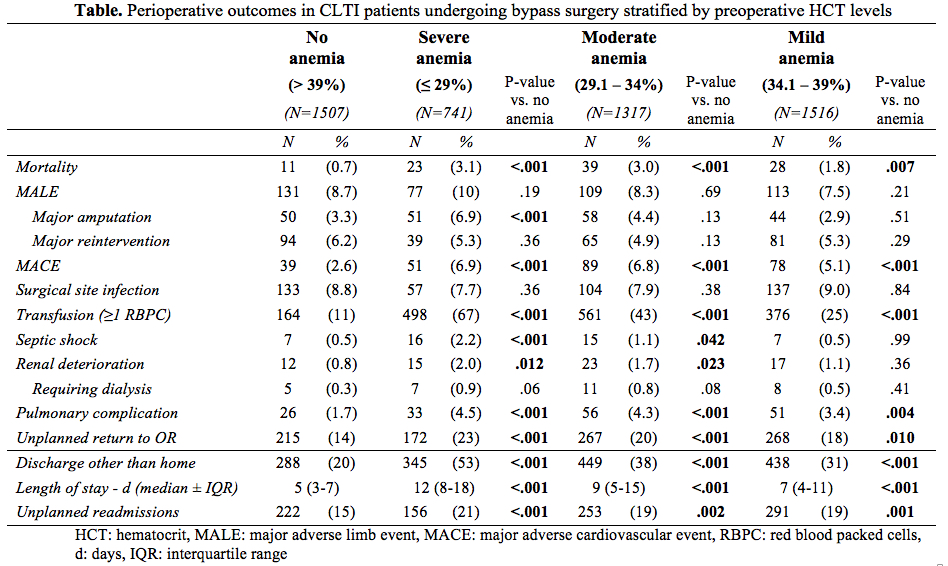
Back to 2017 Karmody Posters




