Perioperative Outcomes of Primary Bypass versus Primary Endovascular Intervention in Infrainguinal Arterial Disease
Thomas C.F. Bodewes, MD, Jeremy D. Darling, BA, Alexander B. Pothof, MD MSc, Sarah E. Deery, MD, Thomas F. O'Donnell, MD, Katie E. Shean, MD, Frans L. Moll, MD PhD, Marc L. Schermerhorn, MD.
Beth Israel Deaconess Medical Center, Boston, MA, USA.
OBJECTIVES: The optimal approach to revascularization remains uncertain for many patients with peripheral artery disease. The purpose of this study was to assess perioperative outcomes of patients undergoing primary treatment for infrainguinal lesions using a national representative clinical registry.
METHODS: Patients undergoing non-emergent primary infrainguinal revascularization were identified in the Targeted Vascular NSQIP 2011-2014. Stratified by symptom status (chronic limb-threatening ischemia [CLTI] and claudication), patients undergoing primary bypass were compared to those undergoing primary endovascular intervention. Patients with prior ipsilateral interventions and those with hybrid procedures were excluded. Multivariable logistic regression was used to establish independent associations between primary procedures and perioperative outcomes.
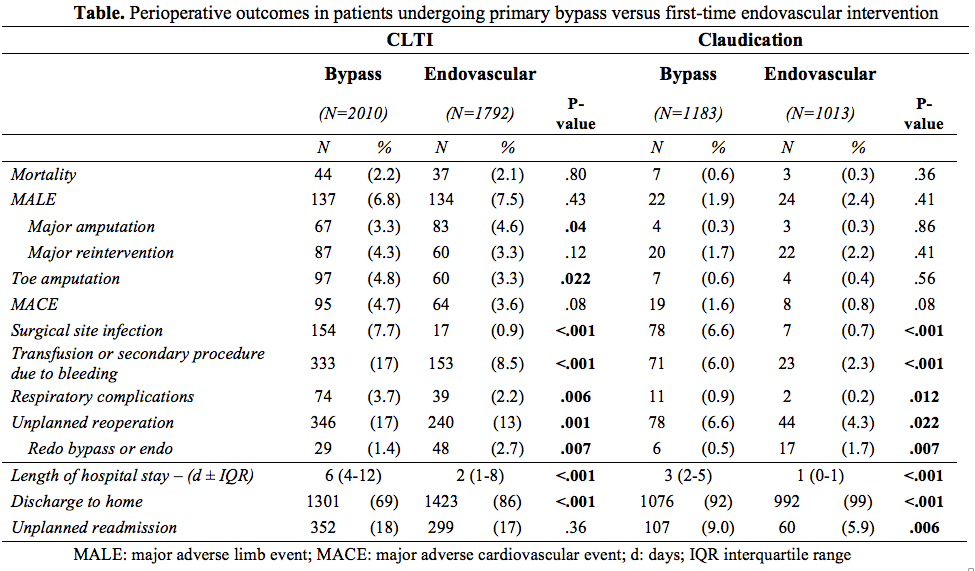
RESULTS: Of 5998 infrainguinal revascularizations performed, 3193 were primary bypass procedures (63% CLTI) and 2805 first-time endovascular interventions (64% CLTI). Patients undergoing primary endovascular intervention were older and had a greater burden of comorbidities. Comparing primary bypass to endovascular intervention, there was no difference in 30-day mortality in CLTI (2.2% vs. 2.1%, P=.80) and claudication patients (0.6% vs. 0.3%, P=.36; Table). Among CLTI patients, primary bypass was associated with toe amputation (4.8% vs. 3.3%, OR:2.0, 95% CI:[1.4-2.9]), MACE (4.7% vs. 3.6%, OR:1.6[1.2-2.3]), surgical site infection (7.7% vs. 0.9%, OR:8.4[5.0-14.1]), transfusion or secondary procedure due to bleeding (17% vs. 8.5%, OR:2.6[2.1-3.2]), unplanned reoperation (17% vs. 13%, OR:1.5[1.3-1.9]), and unplanned readmission (18% vs. 17%, OR:1.3[1.1-1.5]). Patients with claudication undergoing primary bypass had an increased risk of MACE (1.6% vs. 0.8%, OR:2.6[1.1-6.3]), surgical site infection (6.6% vs. 0.7%, OR:11.3[4.8-26.1]), transfusion or secondary procedure due to bleeding (6.0% vs. 2.3%, OR:3.3[2.0-5.5]), unplanned reoperation (6.6% vs. 4.3%, OR:1.6[1.1-2.4]), and unplanned readmission (9.0% vs. 5.9%, OR:1.8[1.3-2.5]). Additionally, first-time endovascular intervention was associated with redo bypass or endovascular intervention in CLTI (2.7% vs. 1.4%, OR:2.2[1.4-3.6]) and claudication patients (1.7% vs. 0.5%, OR:4.3[1.6-11.9]) compared to primary bypass.
CONCLUSIONS: Patients with CLTI and claudication undergoing primary infrainguinal bypass had an increased risk of 30-day adverse events; however, first-time endovascular intervention was associated with redo procedures. Despite likely confounding by extent of arterial lesions, wound severity, and infection, as well as a lack of long-term outcomes, these short-term data are a useful adjunct to help guide decision-making.
Back to 2017 Karmody Posters




