Comparison of the SVS WIfI classification system and the PREVENT III risk score in patients undergoing first-time infrainguinal bypass for chronic limb-threatening ischemia
Jeremy D. Darling, B.A., Katie E. Shean, M.D., Matthew Dernbach, B.S., Thomas F. O'Donnell, M.D., Alexander B. Pothof, M.Sc., M.D., Raul J. Guzman, M.D., Mark C. Wyers, M.D., Allen D. Hamdan, M.D., Marc L. Schermerhorn, M.D..
Beth Israel Deaconess Medical Center, Boston, MA, USA.
OBJECTIVES: Clinical decision-making and more accurate outcome comparisons in chronic limb-threatening ischemia (CLTI) require improved and standardized staging systems. The SVS WIfI classification system and the PREVENT III (PIII) risk score were engineered to predict 1-year amputation risk and amputation-free survival (AFS) after surgical revascularization. This study sought to compare these two prominent staging systems. METHODS: We reviewed all limbs undergoing a first-time infrainguinal bypass for CLTI at our institution from 2005-2014. Limbs were organized into SVS WIfI clinical stages (1 to 4), PIII classification risk scores (low, medium, high-risk), and WIfI mean score stratifications (low, medium, high-risk). Outcomes included major amputation, major adverse limb events (MALE), AFS, and mortality. Outcomes were evaluated using Chi Squared, Kaplan-Meier, and logrank analyses. RESULTS: Of the 1,336 first-time procedures performed, 468 limbs underwent an open surgical bypass (32% rest pain, 68% tissue loss) and were sorted into WIfI clinical stages 1-4 (1%, 34%, 22%, 44%, respectively), PIII risk scores low-risk to high (32%, 51%, 17%, respectively), and WIfI mean score stratifications low-risk to high (48%, 44%, 8%, respectively). An increasing PIII risk score was associated with increased 30-day mortality (P=.03), while an increasing WIfI clinical stage was associated with increased 30-day MALE (P=.046) and increased hospital length of stay (LOS; P<.001). The WIfI mean score stratification illustrated more gradual and more significant differences in both 30-day MALE (P<.001) and hospital LOS (P<.001). Among PIII risk scores, Kaplan-Meier and logrank analyses demonstrated a significant difference in 1-year survival (P<.001), limb-salvage (P=.02), and AFS (P<.001), while the WIfI clinical stages were shown to differ in 1-year limb salvage (P<.001) and AFS (P<.001) (Table I). Ultimately, the WIfI mean score stratification illustrated the most significant differences in 1-year limb salvage (P<.001), freedom from MALE (P=.03), and AFS (P<.01). CONCLUSIONS: Among bypass patients treated for CLTI, PREVENT III risk scores correlate with perioperative and 1-year mortality, whereas WIfI clinical stages and WIfI mean scores strongly predict hospital length of stay and important mid-term limb-related outcomes. These data support a complementary use of the WIfI and PIII staging systems in the management of chronic limb-threatening ischemia.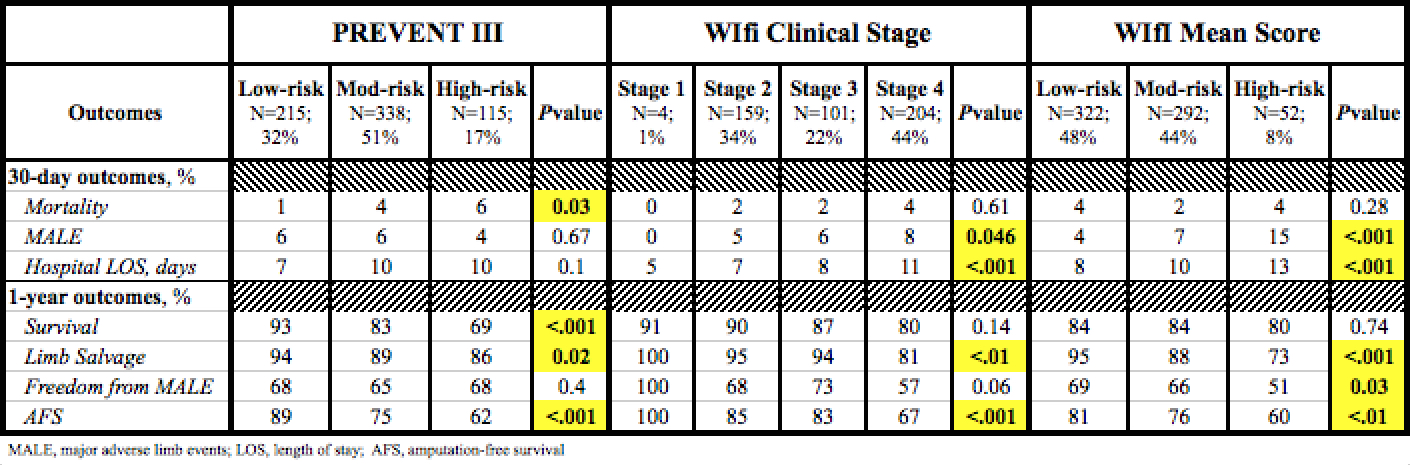
Back to 2017 Karmody Posters




