Early and midterm outcomes after infrainguinal bypass at a tertiary referral center
Harleen K. Sandhu, MD, MPH, Travis Vowels, MD, Charles C. Miller, III, PhD, David Amarodriedger, BS, Samuel S. Leake, BS, Hazim J. Safi, MD, Ali Azizzadeh, MD, Kristofer M. Charlton-Ouw, MD.
McGovern Medical School at UTHealth, Houston, TX, USA.
OBJECTIVES: To evaluate early and midterm outcomes in patients having infrainguinal bypass at a single institution with advanced endovascular capabilities
METHODS: We reviewed the medical records of all patients who had an infrainguinal bypass between August 2004 and October 2015 at our institution. Demographic, operative, and surveillance data were collected for each patient and evaluated using Kaplan-Meier and chi-square analysis.
RESULTS: A total of 351 grafts (polytetrafluoroethylene [PTFE], 112 [32%]; Dacron, 9 [3%]; autogenous vein, 181 [52%], composite, 44 [13%]; and cryopreserved, 5 [1%]) in 320 patients and 340 limbs were included in the present study. Femorofemoral bypasses were excluded. Average age was 60 years (range 7-89) and mostly male (237 [68%]). Sixty-seven (19%) were redo bypasses. Except in cases of trauma, nearly all patients had preoperative attempt at endovascaular repair. Bypass targets were above-knee in 125 (36%) patients, below-knee in 222 (63%), and pedal in 4 (1%). Reason for bypass was acute limb ischemia in 136 (39%) patients, critical chronic limb ischemia (CLI) in 153 (44%), non-critical CLI in 46 (13%), and other in 16 (5%). Early graft thrombosis occurred in 21 (6%) and wound infection in 11 (3%) patients. Overall, limb preservation was successful in 86%. Cumulative 1-year patency for above-knee vs. below-knee bypasses was 70% and 53%, respectively (P < .01) (Figure 1). Predictors of graft failure included the presence of gangrene in the index limb (P=.01; HR 2.29), pacemaker (P=.02; HR 2.17), interposition graft (P=.01; HR 2.08), and prosthetic conduit (P < .01; HR 1.89). Operation for non-critical CLI was protective of graft failure (P=.01; HR 0.42).
CONCLUSIONS:
In patients with critical limb ischemia deemed to be poor candidates for endovascular repair, limb preservation was successful in most patients. Graft patency rates were affected by the high prevalence of redo bypasses, need for prosthetic conduit, and gangrene. Claudication, as opposed to gangrene, was protective of bypass failure and limb loss. These results provide updated outcomes in the "endo first" era.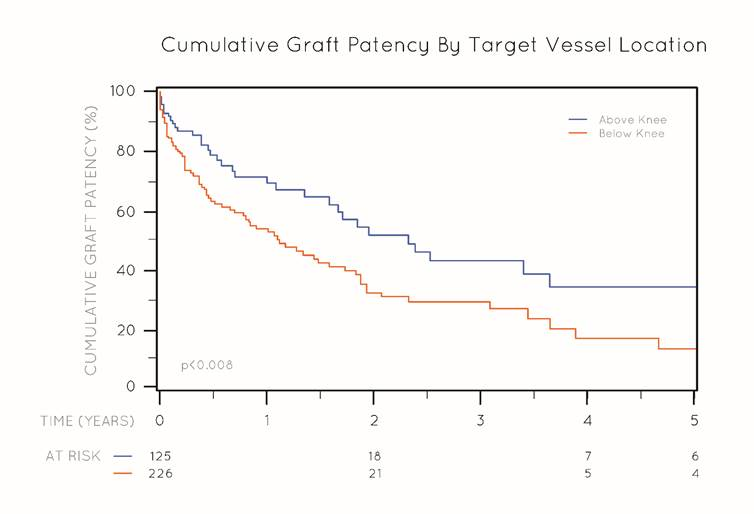
Back to 2017 Karmody Posters




