A Case of Superior Gluteal Artery Pseudoaneurysm Managed by Percutaneous Ultrasound-Guided Thrombin Injection
RATNA C. MEDICHERLA, MD1, Amit R. Shah, MD2, Ross Lyon, MD2, Josef Toussaint, MD2, Aksim Rivera, MD2.
1Montefiore Medical Center, Bronx, NY, USA, 2Jacobi Medical Center, Bronx, NY, USA.
OBJECTIVES:
Gluteal artery aneurysms are very rare, and the majority of reported cases are traumatic pseudoaneurysms (PSA). We report a case of a 62 year-old man who developed superior gluteal artery (SGA) PSA as a complication of bone marrow biopsy, which was treated with percutaneous ultrasound-guided thrombin injection (UGTI).
METHODS:
Patient had a history of von Willebrand disease, cold agglutinins, and newly diagnosed chronic lymphocytic leukemia, which was confirmed on bone marrow biopsy of the right posterior iliac crest. Nine days post procedure, he presented to the Emergency Department with progressively worsening right buttock pain and new onset numbness and tingling in the right leg. Physical exam revealed a tender scab at the entry site of the biopsy needle. He was neurologically intact with palpable pulses throughout. A contrast enhanced computed tomography demonstrated a 4.2cm PSA arising from the SGA in the right piriformis muscle with surrounding hematoma. A duplex ultrasound (DUS) confirmed the diagnosis.
RESULTS:
With the patient in prone position, access to the PSA was obtained using an 18-gauge pericardial needle inserted through the right buttock under ultrasound guidance, and 2,000 units of recombinant thrombin were injected. Manual compression was performed with immediate cessation of flow in the PSA and patent SGA confirmed under DUS. Symptoms improved with alleviation of pain and resolution of numbness and tingling. DUS repeated the next day showed resolution of the PSA with residual hematoma and preserved flow in the SGA. Patient had an uneventful hospital course and was discharged home. He was noted to be doing well on follow-up visits.
CONCLUSIONS:
Gluteal artery PSAs usually present with nonspecific pain/swelling of the buttock or radicular pain due to sciatic nerve compression. Since these lesions often present with gluteal swelling which may be mistaken for an abscess, proper diagnosis by imaging is important to avoid disastrous consequences. Historically, two treatment modalities have been employed in managing these lesions: open surgery and endovascular techniques. In a few case reports, UGTI has been utilized as a less invasive alternative. We present a case of a SGA PSA due to iatrogenic injury successfully managed with UGTI.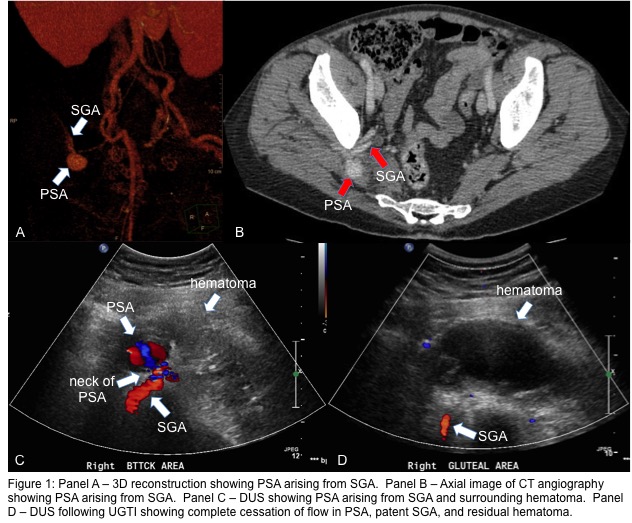
Back to 2017 Karmody Posters




