Symptomatic Abdominal Aortic Aneurysms have Increased Perioperative and Long-term Mortality Risk
Peter A. Soden, MD1, Sara Zettervall, MD1, Katie Shean, MD1, Sarah Deery, MD1, Philip Goodney, MD2, Randall DeMartino, MD3, Marc Schermerhorn, MD4.
1Beth Israel Deaconess Hospital, Newton, MA, USA, 2Dartmouth-Hitchcock Medical Center, Hanover, NH, USA, 3Mayo Clinic, Rochester, MN, USA, 4Beth Israel Deaconess Hospital, Boston, MA, USA.
Objectives: Reports on mortality risk of symptomatic abdominal aortic aneurysms (AAA), compared to elective repair, have been conflicting. The purpose of this study is to quantify perioperative and long-term mortality risk associated with symptomatic aneurysms and to identify risk factors associated with increased mortality in the symptomatic population. Methods: We identified all AAA repairs in the Vascular Quality Initiative (VQI) from 2003 to 2016. We compared 30-day and long-term mortality for asymptomatic, symptomatic, and ruptured AAA repair, stratified by type of repair, endovascular (EVAR) and open. Multivariable logistic regression, Kaplan-Meier analysis, and Cox proportional hazards models were utilized. Results: We identified 32,023 AAA repairs, including 26,403 elective (80% EVAR), 2,872 symptomatic (72% EVAR), and 2748 ruptured (50% EVAR). Compared to elective repairs, patients with symptomatic AAA were younger (72 vs. 73, P < .001) and more often female (25% vs. 20%, P < .001) and non-white (14% vs. 8%, P < .001). Patients with symptomatic AAA were less likely to be on a statin and antiplatelet regimen preoperatively (42% vs. 54%, P < .001) and had larger aneurysm diameters compared to elective repairs (EVAR: 6.1 cm vs. 5.6 cm, P < .001; open 6.8 cm vs. 5.9 cm, P < .001). Thirty-day mortality was increased in symptomatic compared to elective patients (EVAR: 3.4% vs. 0.9%, P < .001; Open: 5.3% vs. 3.0%, P = .001) and was decreased compared to ruptured patients (EVAR: 3.4% vs. 23%, P < .001; Open: 5.3% vs. 35%, P < .001). On adjusted analysis, symptomatic compared to elective patients were at increased risk for 30-day mortality (EVAR: OR 3.0, 95% CI 2.2-4.1; open: OR 1.6, 95% CI 1.1-1.9) and long-term mortality (EVAR: HR 1.6, 95% CI 1.4-1.8; open: HR 1.5, 95% CI 1.2-1.8). Risk factors for 1-year mortality in symptomatic aneurysms included: age, CHF, COPD, CRI, IDDM, and lack of antiplatelet and statin on discharge. Conclusion: Patients with symptomatic AAAs are at increased risk for mortality after open and endovascular repair, both within 30-days and long term. Further investigation is needed to understand why women and non-white patients more often present with symptoms.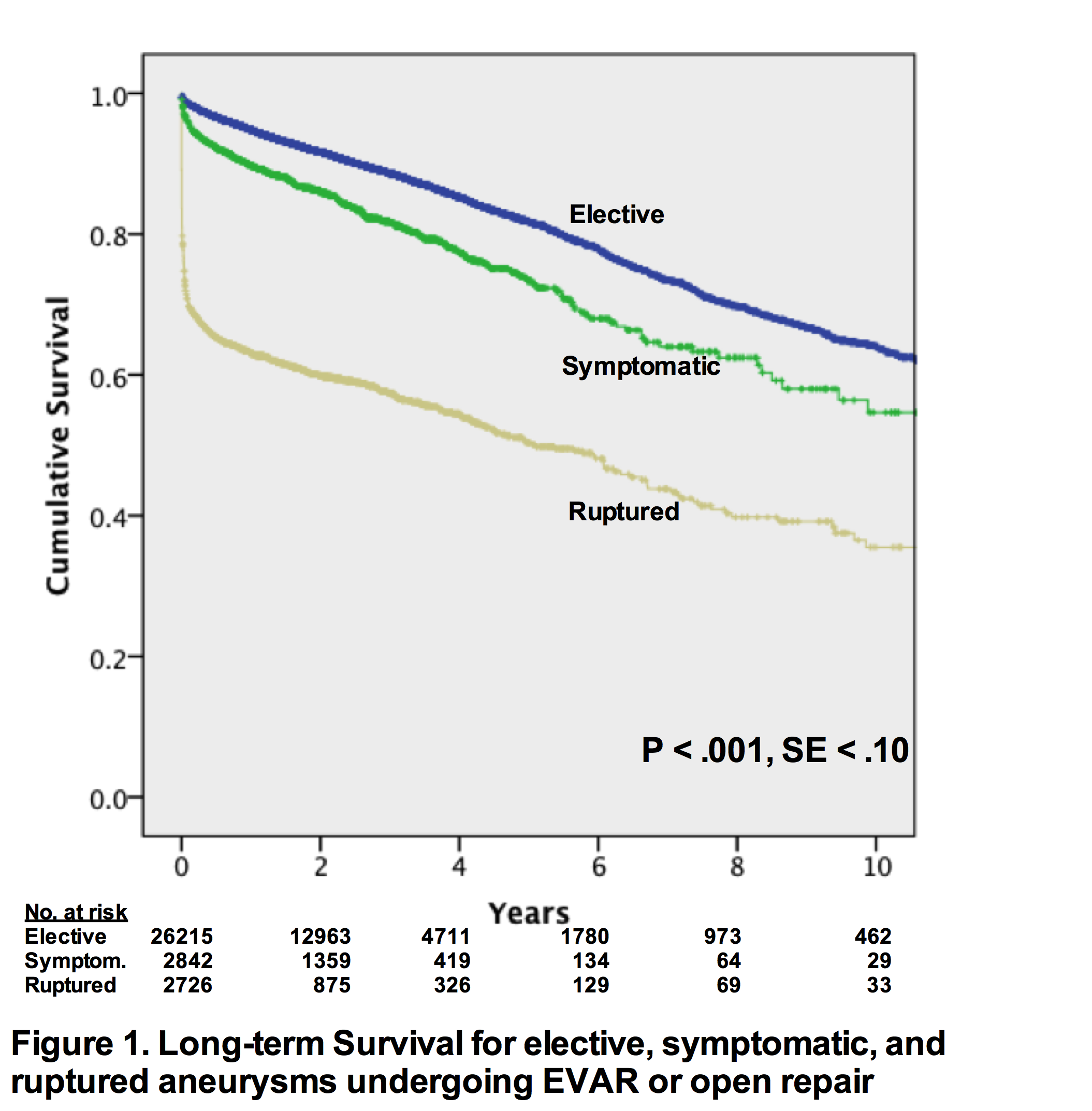
Back to 2017 Karmody Posters




