DE NOVO PARAVISCERAL AORTIC MURAL THROMBUS IN NORMAL APPEARING AORTA: REPORT OF 2 CASES AND REVIEW OF THE LITERATURE
Mariano Arosemena, MD, Paul DiMuzio, MD, Babak Abai, MD, Dawn Salvatore, MD.
Thomas Jefferson University Hospital, Philadelphia, PA, USA.
OBJECTIVE - Aortic mural thrombus is typically associated with a preexisting aortic wall abnormality such as aortic aneurysm and atherosclerosis. Spontaneous non-occlusive aortic thrombus in a normal aorta is uncommon and even rarer at the paravisceral aortic segment. Hence, there are not well-established treatment guidelines.
METHODS - We report two cases of primary paravisceral aortic mural thrombus managed with direct open aortic thrombectomy via a left retroperitoneal thoracoabdominal approach, both with normal appearing aortas.
RESULTS - There are 295 aortic mural thrombi cases reported. The majority are associated with an underlying disease process. Only seven reported cases of de novo paravisceral aortic thrombi with clinically unidentifiable causes are available in the literature. Six were treated by open thrombectomy with sustained primary patency and one was treated with anticoagulation only. The latter had recurrent Superior Mesenteric Artery embolization requiring emergent open embolectomy. We report two female patients who presented with acute onset abdominal pain. CTA revealed paravisceral aortic mural thrombus with insignificant scattered atherosclerotic plaque and no aortic wall abnormalities in both patients. They were initially heparinized and treated with open direct aortic thrombectomy via a left retroperitoneal thoracoabdominal approach. Post-operative courses were uncomplicated with resolution of abdominal pain, and both were released on long-term anticoagulation and low dose aspirin. Clinically appropriate hypercoagulable work up was negative. At three months (Patient 1) and one year follow up (Patient 2), both patients continue to do well and are symptom free with follow-up CTAs showing patent aortas.
CONCLUSIONS - Our review of the literature indicates that de novo paravisceral aortic mural thrombus is a rare condition without algorithm treatment guidelines. Based on our analysis and our two cases, direct open surgical thromboembolectomy should be the primary treatment for symptomatic patients with normal or minimally atherosclerotic aorta, especially in younger patients with low surgical risk and potential for higher rate of recurrence. Anticoagulation as sole therapy carries higher complication rate of end organ distal embolization as compared to open aortic surgery. Such patients should also undergo hypercoagulable workup with anticoagulation initiated at presentation, continued postoperatively, with indefinite anticoagulant and/or antiplatelet therapy, possibly lifelong.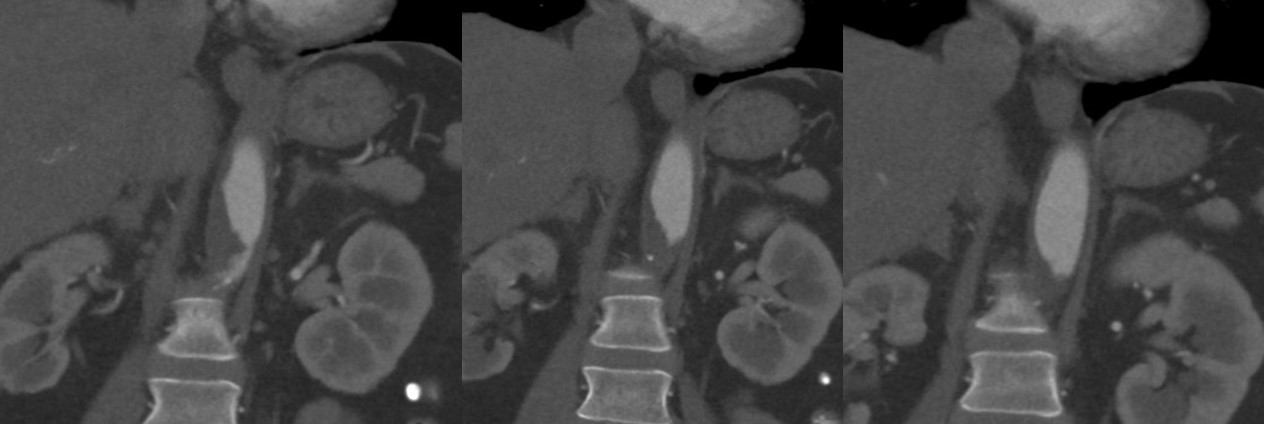
Back to 2017 Karmody Posters




