Single Institution Experience of Tibial Bypass with Autologous and Nonautologous Conduit
John Futchko, MD, Charles DeCarlo, MD, John Phair, MD, Eric Trestman, MD, Evan Lipsitz, MD, Michael Vitti, MD, Francis Porreca, MD.
Montefiore Medical Center, Bronx, NY, USA.
OBJECTIVES:
While greater saphenous vein (GSV) remains the conduit of choice for below-knee bypass, there remains a need to investigate the role of nonautologous conduits (NAC), including those modified with vein cuffs, as a practical conduit option. This study reports our distal tibial bypass experience with multiple conduits types for patients with critical limb ischemia.
METHODS:
We performed a retrospective review of our institutional database for patients undergoing infrapopliteal bypass from January 2009 through December 2015. Bypasses were categorized by graft type as GSV or NAC. Primary endpoints were major amputation free survival and primary graft patency within the first year. A stepwise cox regression model was performed to adjust for confounding demographic variables.
RESULTS:
A total of 245 tibial bypasses in 201 patients were recorded; 102 (41.6%) were single-segment GSV and 143 (58.4%) were NAC. Primary patency at one year was 56.2% (CI 0.466-0.678) for the GSV group and 38.7% (CI 0.311-0.482) for the NAC group. Amputation-free survival at 1- and 2-years was 66.4% (CI 0.578-0.763) and 56.6% (CI 0.475-0.673), respectively, for the GSV group; 64.6% (CI 0.571-0.761) and 55.3% (CI 0.474-0.645) for the NAC group. Subgroup analysis within the NAC cohort revealed 1-year primary patency and amputation-free survival of 41.5% (CI 0.312-0.559) and 71.6% (CI 0.618-0.830), respectively, for heparin-bonded PTFE grafts; 46.9% (CI 0.331-0.663) and 61.9% (CI 0.483-0.793) for PTFE grafts with Tyrell vein cuffs. In Cox analysis, GSV graft predicted primary patency (HR 0.604; P=0.011; 95% CI, 0.411-0.889) when compared to NAC. There was no significant difference in amputation-free survival between conduit types. Of note, amputation-free survival was predicted by medium-intensity (HR 0.599, P=0.017, 95% CI, 0.393-0.913) and high-intensity statin therapy (HR 0.389, P<0.001, 95% CI, 0.236-0.642). 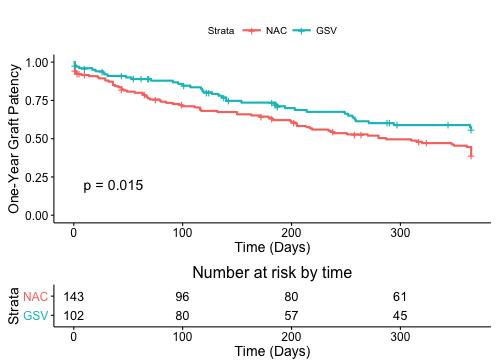
CONCLUSIONS:
GSV offers improved patency for tibial bypasses compared to NAC, however both conduits provided similar rates of amputation-free survival. While GSV remains the optimal conduit, NAC is a reasonable option if GSV is insufficient and limb salvage is the goal. NAC modifications, including heparin-bonded PTFE and Tyrell vein cuffs, offer a modest but nonsignificant benefit in patency. Medium- and high-intensity statin therapy in patients predict improved amputation-free survival.
Back to 2017 Program




