Redo Lower Extremity Bypass has Superior 30-day Outcomes After Failed Ipsilateral Bypass for Critical Limb Ischemia in a Large US Cohort
J. Hunter Mehaffey, MD, Robert B. Hawkins, MD, Anna Z. Fashandi, MD, Megan C. Tracci, MD, JD, John A. Kern, MD, Irving L. Kron, MD, Gilbert R. Upchurch, MD, William Robinson, MD.
UVA, Charlottesville, VA, USA.
Background: Lower extremity bypass (LEB) and infrainguinal endovascular intervention (IEI) are options to treat critical limb ischemia (rest pain/tissue loss) after a failed prior lower extremity bypass but the outcomes are poorly described. The purpose of this study was to compare 30-day Major Adverse Limb Events (MALE) and Major Adverse Cardiovascular Events (MACE) after LEB and IEI in patients with a failed prior ipsilateral LEB and determine associated risk factors.
Methods: Patients with prior failed ipsilateral LEB who underwent LEB or IEI involving the same arterial segment for critical limb ischemia were identified in The National Surgical Quality Improvement Program (NSQIP) Vascular Targeted File (2011-2014). LEB with optimal conduit (single segment saphenous vein) was compared to LEB with suboptimal conduit (prosthetic/spliced vein/composite), and IEI. Primary outcomes were 30-day MALE (Untreated Loss of Patency, Re-intervention, Amputation) and MACE (Stroke, Myocardial Infarction, death). Multivariate analysis was utilized to identify independent predictors of MALE and MACE.
Results: Among 8,066 revascularizations perfomed for CLI, 1,606 (461 IEI, 518 optimal conduit, 627 suboptimal conduit) were performed after failed ipsilateral LEB involving the same arterial segment . MALE was significantly different between between groups (IEI:15.8%, LEB optimal conduit:10.8%, LEB suboptimal conduit:15.5%, p=0.03).The 30-day amputation rate was highest after IEI (IEI:7.8%, LEB optimal conduit:3.7% LEB suboptimal conduit:5.3%, p=0.02). Independent predictors of MALE include transfer from another hospital(OR 1.7, p=0.01), tobacco use (OR 1.5, p=0.02), infrageniculate revascularization (OR 1.6, p=0.004), and optimal conduit (OR 0.5, p=0.002). MACE was also different between groups (3.9% e, 2.7% optimal conduit, 5.6% suboptimal conduit, p=0.049), with no difference in 30-day mortality (p=0.53). Independent predictors of MACE included congestive heart failure (OR 3.0, p=0.01) and dialysis dependence (OR 2.5, p=0.02).
Conclusions: In patients with critical limb ischemia after failed ipsilateral LEB of same arterial segment, LEB with single segment saphenous vein independently reduced MALE and represents the optimal method of revascularization when feasible. Patient comorbidities, not the method of revascularization approach, predicted MACE. High 30-day MALE and MACE highlights the need for improved primary and secondary revascularization strategies as well as the need careful patient selction for revascularization after failed bypass in CLI. 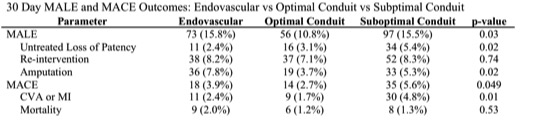
Back to 2017 Program




