Comparison of Early and Late Postoperative Outcomes after Open Supra-inguinal Bypass
Mohammad H. Eslami, MD, MPH1, Denis V. Rybin, PhD2, Gheorghe Doros, PhD2, Jeffery Siracuse, MD3, ALik Farber, MD3.
1University of Pittsburgh Medical School, Pittsburgh, PA, USA, 2Boston University School of Public Health, Boston, MA, USA, 3Boston University School of Medicine, Boston, MA, USA.
Comparison of Early and Late Postoperative Outcomes after Open Supra-inguinal Bypass Operations
Mohammad H. Eslami, Jeffrey J. Siracuse, Denis Rybin, Gheorghe Doros, Alik Farber
Objectives: The choice for open surgical revascularization for aortoiliac occlusive disease (AIOD) is often tempered by patient’s comorbidities. In this study, we set to compare perioperative outcomes as well as association of the choice of operation with 1-year major adverse limb event -free survival (MFS) and 5-year mortality.
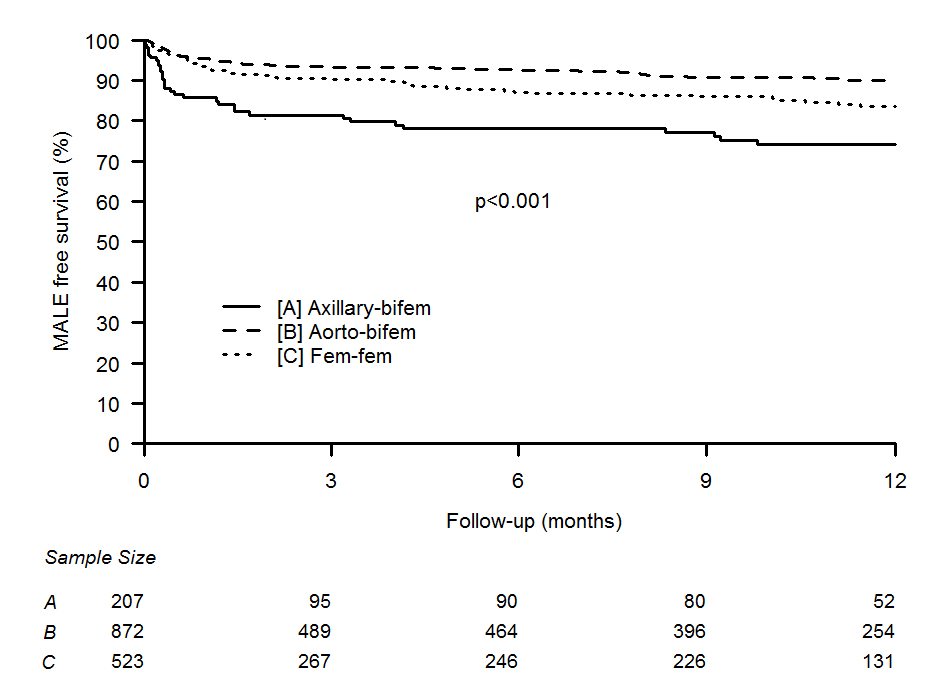
Methods: The Vascular Study Group of New England (VSGNE) dataset for supra-inguinal bypass operations was queried. Patients were divided into three groups; aortobifem (AOB), axillary-bifem (AXB), and femorofemoral (FFB) bypass. Postoperative adverse outcomes, as well as 30-day postoperative death (POD) were compared across three groups using both univariate and multivariate analyses. 1-year MSF were compared with log-rank test and the Kaplan-Meier plot, respectively. Proportional hazard Cox regression was used to compare MFS and 5-year survival.
Results: 1613 cases were included in this analysis (2009-2015); 207 (12.8%) AXB, 883 (54.7%) AOB, 525 (32.5%) FFB. Overall AXB patients were older, and had higher rates of comorbidities than other patients. Rate of postoperative cardiac , respiratory , change in renal function , and composite complications and POD were significantly higher for AXB (p<0.05 for all comparisons). Multivariable analyses (Table 1,* indicates p<.05) suggest that AXB and AOB independently increased the odds of adverse postoperative outcomes and POD(Table). Adjusted analyses suggest that AXB independently increased the hazards of MALE at one year ( Hazards Ratio (HR): 1.76, 95% CI; 1.12-2.78, p=.014) and 5-year mortality (HR: 1.54, 95%CI; 1.11-2.41, p=.009). At one year, FFB and AOB had 1-year MFS and significantly better than AXB (Figure).
Conclusions: Adjusting for all the confounding variables, FFB leads to significantly lower rates of complications and should be the operation of choice among high risk patients with AIOD. Given the similar 1- year MFS and higher complications of AOB, AOB should be selectively performed in low risk patients only.
| Contrast | Cardiac Complications | Respiratory Complications | Change in Renal Function | Composite complications | 30-day Mortality |
| Odds Ratio, 95% Confidence Interval | Odds Ratio, 95% Confidence Interval | Odds Ratio, 95% Confidence Interval | Odds Ratio, 95% Confidence Interval | Odds Ratio, 95% Confidence Interval | |
| AOB vs. FFB | 3.23, 1.48-7.026* | 5.47, 2.80-10.67* | 3.18, 1.754-5.781* | 4.18, 2.86-6.11* | 1.37, 0.562-3.37 |
| AXB vs. FFB | 2.41, 1.035-5.65* | 2.60, 1.22-5.56* | 1.82, 0.94-3.84 | 2.78, 1.79-4.34* | 3.497, 1.65-7.41* |
Back to 2017 Program




