Active Tobacco Use In Patients With Claudication Does Not Affect Outcomes Following Endovascular Interventions
Ian Schlieder, DO, Michele Richard, MD, Alpen Nacar, MD, Rebecca Rieger, MD, Alan Dietzek, MD.
Danbury Hospital, Danbury, CT, USA.
OBJECTIVES In the present endovascular era, the indications for intervention in claudicants have become less strict. Many interventionalists, however, will not intervene on patients with life style limiting claudication unless they have discontinued tobacco use. Many patients are unable to comply with this goal and there is little published evidence to suggest that continued tobacco use results in poorer outcomes. We sought to determine if it is justified to deny this group of patients endovascular, potentially life style improving, procedures based upon their outcomes.
METHODS Retrospective chart review was performed between 2007-2011 at a midsize community teaching hospital. Patients included had documented lifestyle limiting claudication, underwent endovascular therapy and who had no previous vascular intervention. We divided the patients into 2 groups: active smokers (AS) and non-smokers (NS) including former and never smokers. Outcome variables included number of reinterventions, time to reintervention and or surgical revascularization, limb loss, MI, stroke and death.
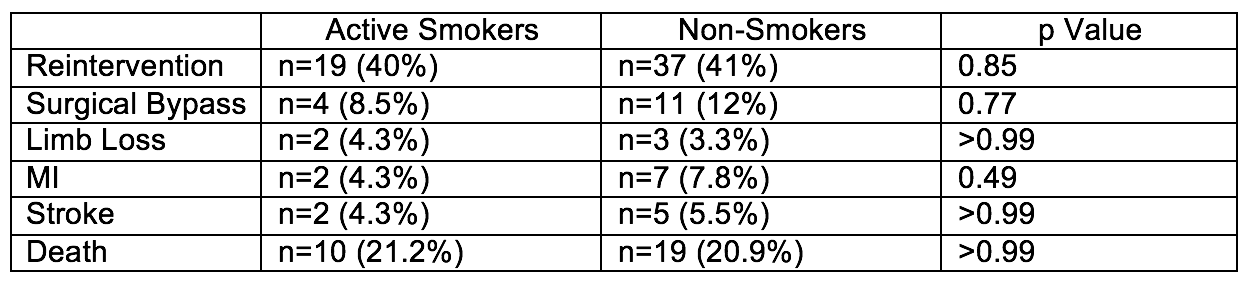
RESULTS 138 patients met inclusion criteria. 47 (34%) were active smokers versus 91 (66%) who were non-smokers. Mean age at initial intervention was 66.34 years (SD 10.7) with 89 being male (64.5%). Mean follow up was 3.6 years and was not significantly different between the two groups. Between the two groups (AS vs NS) there was no statistically significant difference between the rate of reintervention, surgical bypass, limb loss (chart). We also saw no difference in rate of MI, stroke or death during our follow up period.
CONCLUSIONS Although tobacco use has been shown to negatively impact bypass patency our data shows that it does not appear to increase the rate of reinterventions, conversion to open surgical revascularization, limb loss, or other morbidities in patients undergoing endovascular interventions for claudication. We continue to strongly recommend to all of our patients who smoke the discontinuation of tobacco use. We do not believe, however, that those patients that are unable to quit should be denied the potential benefit of an endovascular intervention. The most important limitation of our study is the small numbers of patients available for review. Larger studies will be necessary to confirm our findings.
Back to 2017 Program




